Flap Surgery. Materials for Osteogingivoplasty
Machine translation
Original article is written in RU language (link to read it) .
Osteogingivoplasty is a type of flap surgery that involves the use of agents aimed at stimulating reparative mechanisms in the bony structures of the periodontal apparatus.
Unique training from leading specialists in the treatment of periodontal tissue diseases is presented in the online course Masterclass in Surgical Periodontology: Techniques and Innovations.
After performing surgical sanitation of the pathological periodontal pocket, a blood clot is formed, which serves as a temporary matrix for subsequent transformation first into granulation tissue, and then into scar tissue, or, if the course is favorable, regeneration of all structural components of the periodontium, including bone tissue, is observed.

Figure 1. Filling the socket with transplant material.
In the future, the bone defect may be subjected to inflammation due to the activation of osteoblast function, leading to an increase in collagen synthesis in the bone matrix. Alveolar bone is characterized by active regeneration, during which edge defects can restore up to 70% of the lost volume. However, to activate the processes of bone tissue restoration, regeneration induction is necessary, which is possible against the background of regenerative therapy.
Hegedus first applied allograft in 1923 to replace the lost fragment of the alveolar process, and since then, methods have been developed to increase the activity of bone regeneration after flap surgeries.
At different times, the following substances have been used to stimulate osteogenesis:
- beef bone, subjected to boiling and ground into powder (Beube, Siilvers);
- autogenous crushed bone fragments (Forsberg);
- autogenous and beef bone tissue, subjected to deep freezing and treated with mercurochrome (Kremer).
From the first days of application in the thickness of the spongy autograft, intensive bone formation is initiated under the influence of cells from the autologous bone marrow, which have an increased osteogenic potential. The main drawback of using autologous tissue is the extensive trauma to the donor site, which often exceeds the trauma at the site of the surgical intervention.

Figure 2. The socket filled with the graft.
Modern bone grafts are represented by the following types:
- lyophilized bone, bone meal, chips, cartilage;
- formalinized cartilage, bone.
Formalinized and lyophilized materials create favorable conditions for subsequent prosthetics due to their good processability. Lyophilized grafts are not recommended for use on infected areas. In the presence of periodontal pockets, preference should be given to formalinized grafts, which have an antimicrobial effect due to the release of formaldehyde molecules.
The process of lyophilization of bone tissue leads to a loss of regenerative capabilities. However, effective regeneration during formalinization is observed in 40% of cases, while in the case of lyophilization, it is 75%. The negative impact is attributed to the immunogenic qualities of the grafts, which are more significantly reduced during lyophilic drying but are less affected during formalinization.
In periodontal surgery, the "cultivation" of osteogenic tissue has been widely used in recent years; this process involves placing a hollow implant made of porous titanium nickelide into the spongy substance of the iliac bone.
Structure of the Implant
Two porous hollow tubes of equal size (2-2.5 cm), with a diameter difference of 1 mm, and a wall thickness of 0.3–0.4 mm, are arranged one inside the other. The diameter of the outer tube is 10-15 mm.
The chosen design is explained by the possibility of repeated harvesting and the convenience of extracting the cultivated material.
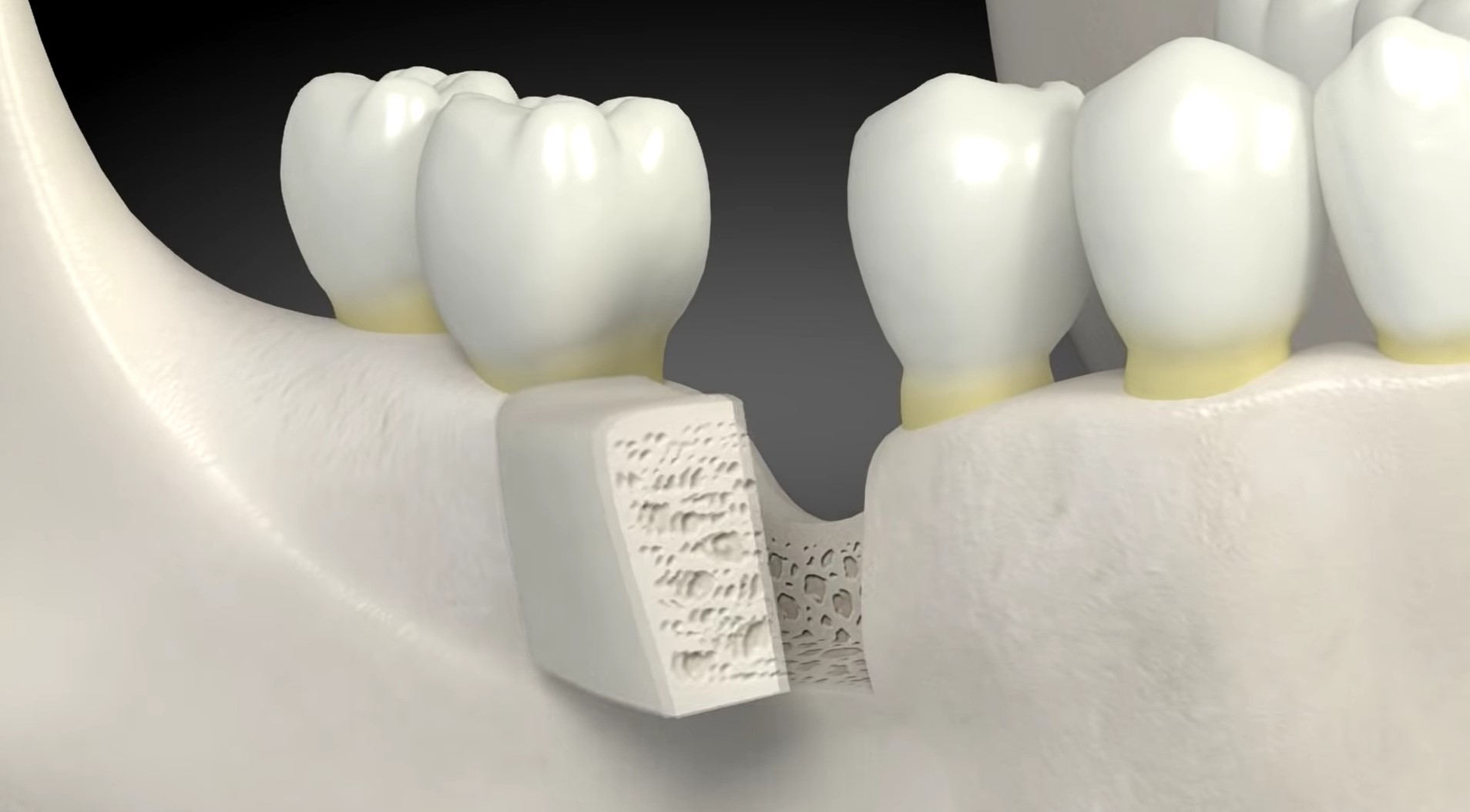
Figure 3. Application of allograft.
After the implantation of the described structure into the bone tissue of the iliac crest, due to tissue diffusion through the porous walls of titanium nickelide, myeloid tissue begins to grow into the "well," which gradually fills it completely. This tissue then transforms into cartilage and subsequently into bone according to the principles of indirect osteogenesis.
The use of osteogenic tissue in surgical periodontology guarantees the formation of a full-fledged regenerate in the bone wound within the next six months, and in some cases even earlier; it all depends on the initial volume of the defect, and bone growth of 4-6 mm can be achieved.
Among the various types of allografts, demineralized bone grafts are distinguished by their high restorative capacity of bone tissue. This is due to the presence of local regulators of osteogenesis:
- skeletal growth factor;
- morphogenetic bone protein.
These osteogenesis regulators trigger the activation of the quantitative and morphological potential of the cells.
The modern production technology is designed in such a way that it allows enriching the preparation with certain medications, including antiseptics and antibiotics, which helps to reduce the bacterial contamination of the donor fragment.
The main disadvantage of this material is its immunogenicity, which causes the development of an inflammatory reaction in the surrounding tissues.
Brefoquity
This material has a simple antigenic structure, which determines its low immunogenicity. Specialists recommend preferring the bone tissue of a human embryo that has reached the age of six months, as by this time the bone material already has a complete structure.
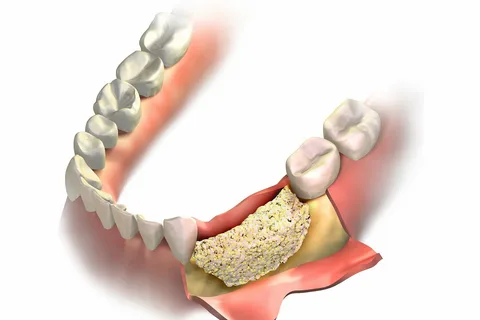
Figure 4. Osteogingivoplasty operation.
Brefoсost contains the following components:
- brefoсhenka;
- cartilage.
This transplant material has plasticity, which allows it to effectively fill a bone defect of any configuration.
The main disadvantage of brefoсost: it often resorbs faster than bone tissue can form.
Collagen-containing materials
They are obtained from the dermis of cattle. The technology for producing solubilized collagen significantly reduces its antigenic properties, but this does not completely eliminate the possibility of an allergic reaction.
Collagen serves as the basis for creating a wide variety of preparations. All of them can tightly seal bone defects, and due to their porous structure, they have a hemostatic effect. The porous structure is also suitable for enriching the transplant with pharmacological agents: antiseptics, antibiotics.
In an inflammatory environment, in the presence of proteolytic systems, collagen destruction occurs and stimulation of reparative regeneration is not observed. To ensure collagen stabilization, hydroxyapatite is added to it, as well as nylon, synthetic fibers that give the composition greater strength.
During regenerative therapy, the following groups of drugs may also be used:
- blood preparations;
- tissue transplants;
- fibers of the antiseptic drug letilan;
- synthetic bone substitutes based on hydroxyapatite.
Hydroxyapatite-based preparations
There are resorbable and non-resorbable hydroxyapatite. The former is a low crystalline substance with high sorption capabilities. The latter is a chemically stable substance that is practically insoluble in water.
Hydroxyapatite can be transformed into a fine-dispersed fraction due to cryogenic treatment during production. Such transplant material allows for the formation of reliable chemical bonds with bone tissue, ensuring the initiation of osteogenesis and cementogenesis processes.
Known materials for osteogingivoplasty are made from a natural substance obtained in the laboratory from algae. This biopolymer is enriched with numerous macro and microelements, contains gels of natural polymers that can form hardening structured tissue: chitin, protein, hyaluronic acid, chondroitin sulfate.

Figure 5. Preparation based on collagen and hydroxyapatite.
This biopolymer contains algigel, and hydroxyapatite is used as an additive. The preparation is characterized by high sorption capabilities, which allows it to retain moisture in the periodontal pocket, providing thermal insulation for it.
There are also preparations that are produced based on type 1 collagen and glycosaminoglycans. They have unique biochemical and physical characteristics. It has been clinically established that their use in the process of comprehensive therapy for periodontitis stimulates the activation of reparative processes both in the bone and in the periodontal apparatus.
More relevant information on this topic can be found in the webinar Surgical Periodontology Without Incisions. "Tissue Stretching Concept".
