Classification of Dental Deposits
Machine translation
Original article is written in RU language (link to read it) .
The pellicle is a structural coating of the tooth that plays a primary role in the development of caries, as the pellicle serves as a foundation for the attachment of cariogenic microorganisms. Understanding the structure of tooth coatings and educating the patient on daily oral hygiene will help reduce the risk of tooth decay.
Method for detecting subgingival tartar: tools and techniques in the webinar Set of non-surgical methods for treating periodontitis.
Structural formations that can be identified on the surface of an erupted tooth:
- the cuticle represents a reduced epithelium of enamel;
- the pellicle is a newly acquired cuticle after the tooth has erupted;
- plaque, seeded with microorganisms and their metabolic products;
- tartar, hardened dental plaque, includes supragingival and subgingival tartar.
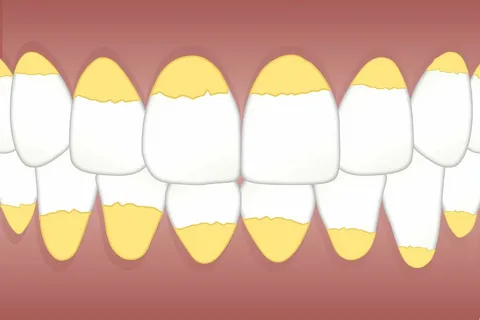
Figure 1. Plaque on the surface of the teeth.
Cuticle
The nasmyth membrane or cuticle is a reduced epithelium of the enamel organ. It does not play a significant role in physiology as it disappears without a trace almost immediately after the tooth erupts, with only isolated patches remaining in the form of a microscopic film on the surface of the enamel, which in rare cases reach the enamel-dentin border.
Pellicle
The pellicle is formed from salivary glycoproteins and represents a tightly adhered film that appears on the surface of the tooth after eruption. The pellicle does not contain microorganisms, but its significance in the attachment of bacteria to the enamel surface is high: the adhesion of S. sanguis to tooth tissues significantly increases if the enamel is lined with pellicle, while in the case of its removal, the adsorption of S. salivarius significantly worsens.
After the removal of the pellicle through abrasive action, it quickly regenerates due to the constant contact of the tooth surface with oral fluid. The state of the pellicle determines the mechanisms of permeability and diffusion on the enamel surface.
The role of the pellicle is important in the process of selective attachment of microorganisms, and consequently, in the formation of dental plaque. In a way, this coating ensures the integrity of the underlying structures of the enamel, but a dense thick layer of pellicle does not indicate the resistance of the enamel. If we study the amino acid composition of this structural coating, we can conclude that the pellicle is an intermediate link between dental plaque and the precipitate of salivary mucin.

Figure 2. Soft and hard dental deposits on teeth.
The condition of the pellicle determines the mechanisms of permeability and diffusion on the surface of the enamel, selective attachment of microorganisms to the tooth tissues.
The pellicle cannot be detected with the naked eye; to identify it in the clinic, dyes (fluorescent dyes, methylene blue) are used. Sometimes it is stained by coloring food pigments, chromogenic bacteria, and medications. Abrasive tools easily remove the pellicle, but it quickly regenerates due to contact with saliva.
The main role of the pellicle in the formation of dental plaque is to create conditions for the initial stage of colonization of pathogenic flora on the enamel surface. Against the background of unsatisfactory hygiene levels, microorganisms begin to attach to the pellicle, forming a layer of plaque. During the examination along the gingival margin, dental plaque is identified on the surface of the teeth, which can be easily removed with regular tooth brushing. Typical locations of dental plaque include pits and fissures, cervical areas, and the space from the edge of the gum to the contact point.
Dental Plaque
Dental plaque is a formation consisting of colonies of microorganisms that are located within a matrix. The latter is formed from proteins, lipids, polysaccharides, and mineral components.
Among the inorganic substances in dental plaque, the largest share belongs to: calcium, phosphates, phosphorus, magnesium, and fluorides. In dental plaque, calcium can bind with phosphates, extracellular proteins, or microorganisms. The concentration of fluoride in plaque increases after the use of fluoride preparations, against the background of consuming water that contains an optimal amount of fluoride ions.

Figure 3. Staining of plaque on teeth.
Dental plaque does not have the ability to adhere as tightly to the surface of enamel as the pellicle does, but it is also not free food debris that can be removed by simple rinsing. The most difficult surfaces of the tooth to clean are the following: pits, fissures, lateral surfaces, and the gingival margin.
Classification of dental plaque based on its localization on the tooth:
- gingival;
- subgingival;
- proximal.
In the pathogenesis of dental caries and periodontal diseases, an important factor is the colonization of microorganisms on the surface of enamel. In young people, the intensity of caries and periodontal diseases directly depends on the volume and distribution of plaque on the teeth. The predominance of soft foods in the diet, along with a preference for consuming mainly easily fermentable carbohydrates, provokes a rapid and significant increase in plaque. Due to its porous structure, dental plaque allows carbohydrates to penetrate easily into the deeper layers.
Types of dental plaque include the following:
- white plaque, characteristic of patients with low hygiene levels;
- green plaque forms as a result of the activity of bacteria that produce chlorophyll;
- brown plaque – this is smoker's plaque, as well as that of patients whose work is related to the production of copper items.

Figure 4. Removal of dental deposits.
Mechanism of dental plaque formation
The onset of dental plaque formation is associated with the adhesion of a monolayer of bacteria to the tooth pellicle. The attachment of microorganisms occurs due to a sticky interbacterial substrate. Plaque formation begins in hard-to-clean areas of the crown: fissures, gingival zones, and contacts.
Biofilm arises due to the adsorption of microorganisms on the surface of the tooth and grows through the gradual layering of bacteria, with the layering occurring in a specific order: first coccal flora, then rod-shaped, and finally filamentous bacteria. When the thickness of dental plaque reaches a significant size, anaerobic forms of microorganisms begin to prevail in it.
The normal microflora of the oral cavity is characterized by a high content of lactobacilli, Str. Mutans, Str. Salivarius, and actinomycetes; under certain conditions, these microorganisms acquire cariogenic characteristics.
The flora of the biofilm begins to build matrix components from the incoming nutrients. Starches, which poorly diffuse into the biofilm, serve as a bacterial substrate. The microorganisms of the biofilm are capable of independently creating extracellular products from the incoming nutrients: dextrans, levans, and glycans.
The properties of the metabolic products of biofilm microorganisms:
- Dextrins have increased adhesive properties, ensuring the attachment of plaque to the tooth enamel, and they release organic acids.
- Levans are a source of nutritional carbohydrates for the microorganisms in dental plaque against the backdrop of the cessation of access to exogenous nutritional components. Levans also contribute to the release of energy, with organic acids being released as a byproduct.
- Glycans promote adhesion between the bacteria themselves, as well as to the surface of the enamel, facilitating the growth and increase of dental plaque.
Biofilm cannot be rinsed away; during tooth brushing, it is not always possible to remove it, and only mechanical scraping during professional hygiene procedures contributes to the removal of dental plaque. Biofilm rapidly forms in the context of consuming soft food, while hard food, which complicates chewing, slows down its formation.

Figure 5. Dental plaque and tartar on the surface of the teeth.
Tartar
The biofilm mineralizes over time and forms tartar.
Characteristics of supragingival tartar
- Typical localization – above the gum line.
- Visible to the naked eye on the surface of the tooth.
- Most often found on the buccal surfaces of molars (at Wharton's duct).
- Color is white, less often whitish-yellow.
- Consistency is hard or clay-like.
- Easily removed from the surface of the tooth by scraping.
- The structure of supragingival tartar is salivary, believed to form from saliva.
- Composed of inorganic (calcium phosphate and carbonate, magnesium phosphate) and organic components.
Characteristics of subgingival tartar
- Characterized by a higher ratio of calcium to phosphorus.
- The amount of sodium increases proportionally with the depth of the periodontal pocket.
- Forms from inflammatory products with the involvement of tissue fluid, desquamated epithelium, and microorganisms from the periodontal pocket.
- Localization – below the marginal gum, on the root cement, detected during careful probing of the pockets.
- Has a hard structure, dark brown or greenish-black color, tightly bonded to the tooth tissues.
- Source of minerals – gingival fluid.
Video protocol of professional hygiene for patients with implants at the webinar Caring for Implants: How to Extend the Lifespan of Implant Restorations - One Cleaning is Not Enough! Part 1.
