Sialography
Machine translation
Original article is written in RU language (link to read it) .
Sialography is a method for diagnosing salivary glands, a radiological examination with a contrast agent, which is part of the mandatory list of studies for patients with salivary gland diseases.
More about sialography in the webinar Radiological Examination in Dentistry.
Oil-based contrast agents
The most popular radiopaque agents for sialography are oil-based: lipiodol, iodipin, ethiodol, iodilipol.

Figure 1. Salivary glands.
Factors that contributed to the widespread use of iodinated oils for sialography:
- excellent radiopacity;
- viscosity that allows radiological examination hours and days after the cannula is removed from the duct system.
Research Methodology
Radiopaque oily preparations are introduced into the gland tissue using a syringe through the excretory duct. A special metal cannula is attached to the syringe. Up to 1.5 ml of oily composition is required to completely fill the ducts of the submandibular gland, while the duct system of the parotid gland holds about 2 ml.
The fullness of the duct system with the preparation can be judged by the emergence of painful discomfort in the patient.
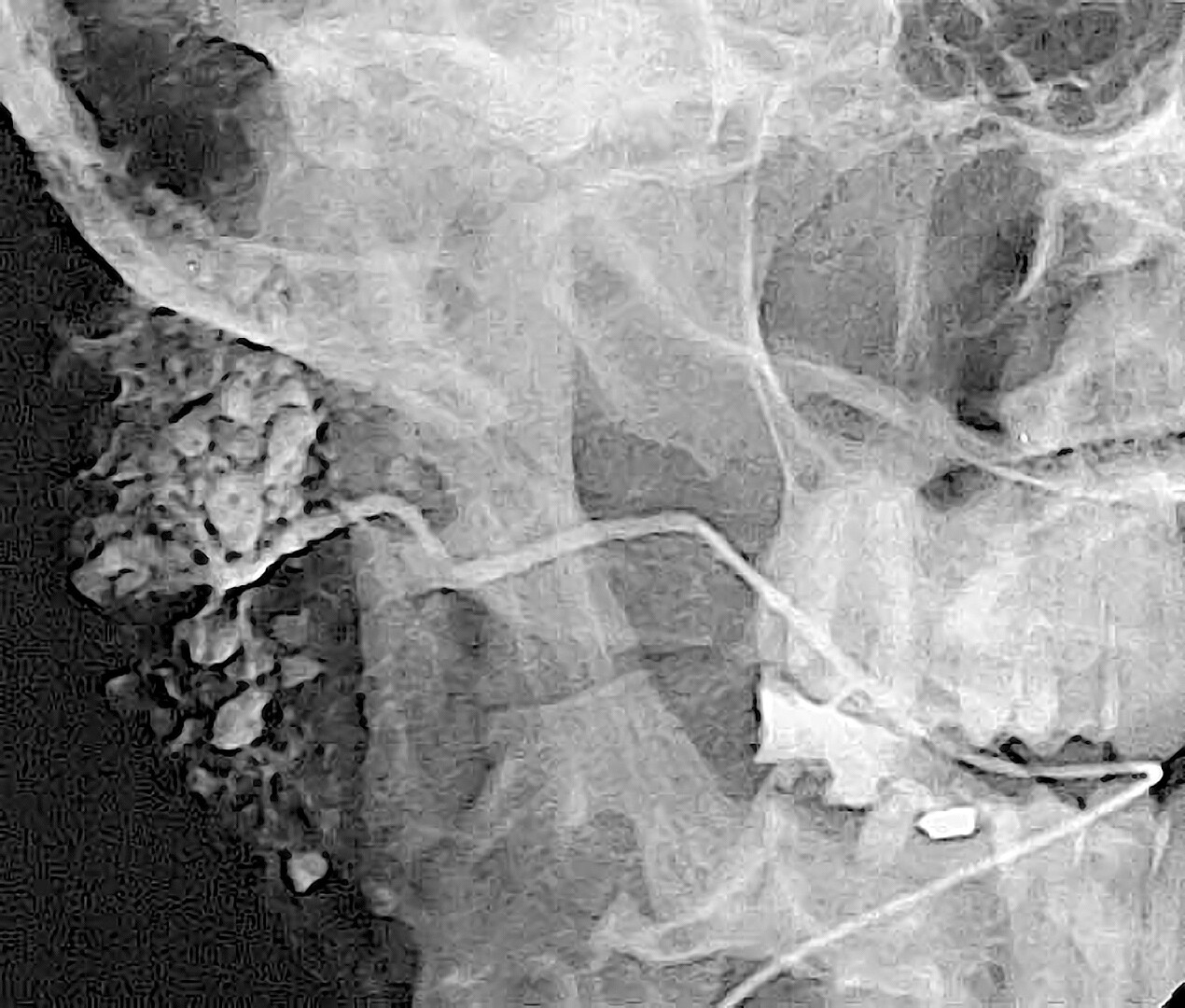
Figure 2. Sialogram.
The disadvantages of this technique for introducing radiopaque agents are:
- it is impossible to assess the pressure with which the agent is injected into the gland, which may not be safe for the gland itself;
- the cessation of the flow of the radiopaque agent upon the onset of pain symptoms is not an objective criterion, as the pain threshold varies significantly among individuals;
- the reliance on the average volume of the radiopaque agent needed to fill the duct system is also not an objective measure, as this volume can vary greatly in either direction, depending on the nature of the inflammatory disease of the gland.
There are some contradictions regarding the effect of oily agents on the parenchyma of the salivary gland. Some specialists emphasize the weak therapeutic effect of these agents immediately after administration, which is due to the disinfecting ability of iodine. However, there is an opinion that radiopaque agents with an oily base are retained by the gland's tissues for an extended period, contributing to the maintenance of inflammation.
A common complication has been the penetration of radiopaque oily compositions into the tissues adjacent to the gland, which can occur due to accidental perforation of the duct wall. This leads to the retention of the composition in the gland's tissues, sustaining inflammation.
In cases of acute pathology of the gland's secretory capacity, the introduction of oily preparations often provokes a more aggressive course of pathological reactions in the future. In such situations, the oily substance is detected on X-rays years after its introduction.
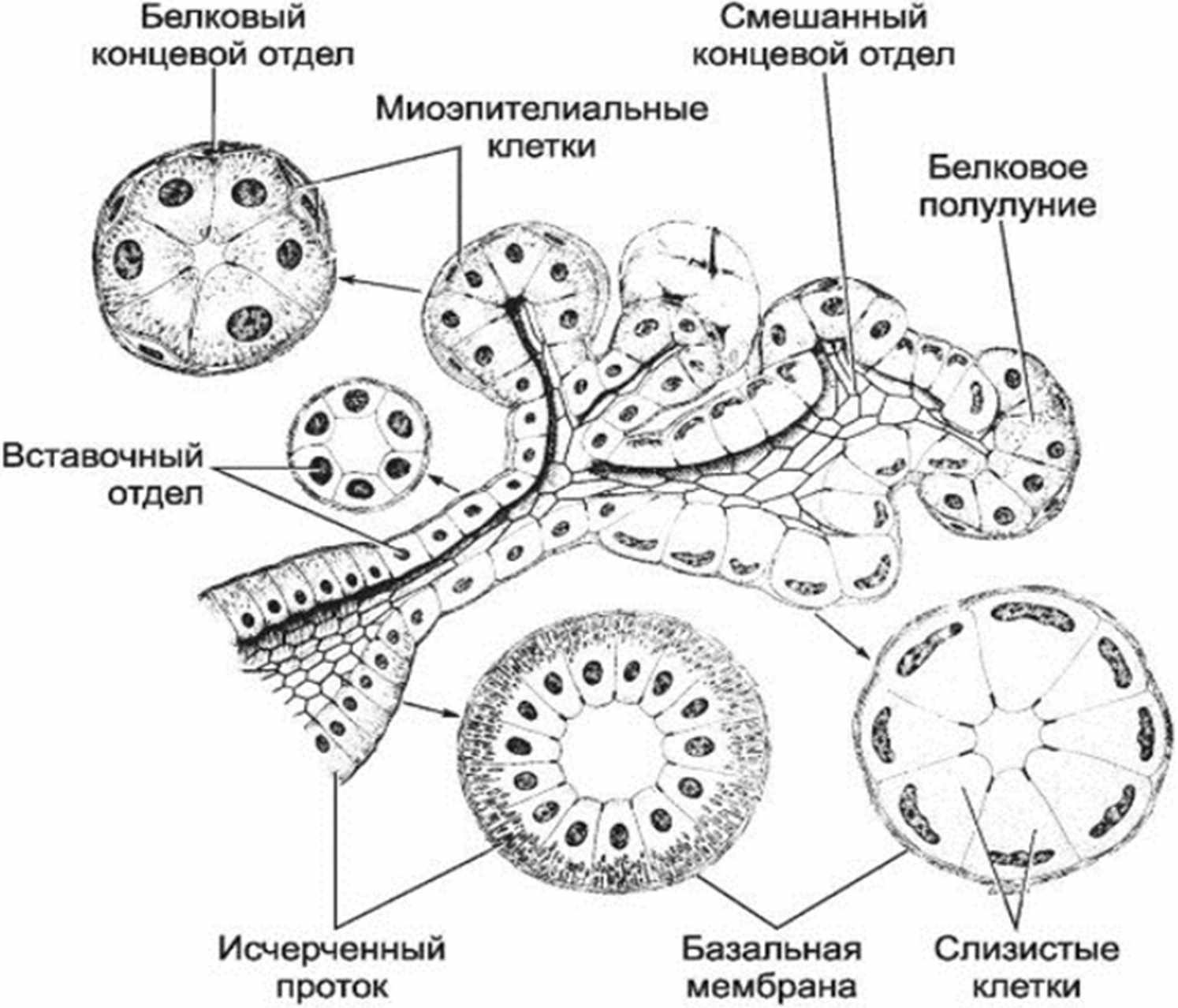
Figure 3. Structure of the salivary gland.
The use of water-soluble compositions with radiopaque properties helps avoid many complications and does not provoke pathological changes in the gland.
Water-soluble radiopaque solutions
Today, the use of water solutions of organic triiodinated compounds is gaining increasing popularity for sialography: urographin, verographin, visotrast, triombrast, urotrost.
Advantages of these solutions
- low toxicity;
- good radiopacity;
- high level of absorptive capacity, which prevents the retention of the drug in the gland with significant impairment of its function.
The main disadvantage of radiopaque water-soluble compositions is their rapid elimination from the gland's tissues, which complicates the acquisition of informative sialograms during the described sialography technique.
The low viscosity of the radiopaque water-soluble preparation when injected with a syringe can provoke the development of excessive, harmful pressure for the gland. In contrast, the use of metal cannulas for injecting water solutions promotes the outflow of the substance from the duct into the oral cavity.
For the introduction of aqueous solutions of radiopaque agents, a proprietary technique has been developed.
The essence of sialography technique is based on the introduction of a justified volume of radiopaque agent into the duct system under controlled pressure, simultaneously performing radiography.
The recommended pressure level for the introduction of the radiopaque composition is about 200 mm Hg, as the gland has the ability to produce secretions against this pressure, making it safe for its tissues.

Figure 4. Conducting sialography.
The new sialography technique requires a conical dilator for the orifice of the main duct, the use of polyethylene catheters or a set of bougies used for dilating the tear ducts is allowed. Catheters can be made independently from polyethylene tubes up to 3 mm in diameter. It is important to sharpen the tip of the catheter; for this, it is heated over the flame of a spirit lamp and then stretched. The required length of the catheter is 10 cm.
Due to its softness, the catheter conforms to the bends of the duct, which prevents perforation of the walls, it closely contacts the walls of the duct, ensuring reliable sealing. To give the catheter sufficient rigidity, a wire mandrel is placed inside it.
Sialography technique using the example of the parotid gland
The patient is seated in the dental chair, and a dilator is inserted into the orifice of the excretory duct. Then, the cheek is pulled forward with fingers. This allows straightening the characteristic bend of the cheek section of the duct for the parotid gland. Next, the dilator is removed, and the soft catheter equipped with a wire mandrel is screwed in with rotational movements.
The mandrel is pulled out during catheter insertion so that the medial tip remains at the level of the orifice, which can be easily monitored through the polyethylene catheter due to its transparency. The length of the mandrel extended from the catheter is used to assess the depth of catheter penetration into the duct. As the mandrel is withdrawn from the catheter, it provides softness to the latter, making it elastic, which protects the duct from damage.
When the catheter is inserted to a depth of about 2 cm into the duct, the mandrel is completely removed, and the catheter is self-secured by the patient using their lips. If the salivary gland is functioning, saliva flows from the catheter. If there is no saliva secretion due to gland disease, the catheter is filled with saline from a syringe. This serves as a preventive measure against air entry and allows for avoiding incorrect assessment of sialograms.
Sialography Technique Using the Example of the Submandibular Gland
The polyethylene catheter is placed in a similar manner when examining the submandibular gland. If the clinical situation does not allow for catheter insertion using the presented technique due to a narrow duct orifice, a nylon thread is first introduced into the duct, which serves as a guide for the catheter. Then, the polyethylene catheter slides along the nylon thread and is gradually inserted into the duct. As soon as the catheter is inserted to a depth of at least 3 mm, the guide is removed, and a wire mandrel takes its place.
If the catheter cannot be inserted into the excretory duct due to the anatomical features of the salivary gland (scarring changes, multiple orifices), a surgical method is used. In this case, the main excretory duct is isolated and a longitudinal incision is made distal to the obstruction. This direction of the incision serves as a prevention of scarring changes. A catheter is introduced through the incision and is fixed with a ligature that is passed around the duct. After the procedure, the ligature is removed.
Once the catheter is inserted, the patient is seated, the device is connected to the catheter, and a pressure of about 200 mm Hg is created. After 15 seconds from the start of the introduction of the contrast agent into the gland, the first image is taken. This corresponds to the filling phase of the gland's duct system.
This image serves to assess the filling of the duct system only. Then the cassette is changed and the next image is taken, approximately one minute after the start of the introduction of the contrast agent. This image corresponds to the filling phase of the gland's parenchyma.
The second image is used to assess the filling of the parenchyma of the salivary gland, provided that it is not damaged by a pathological process.
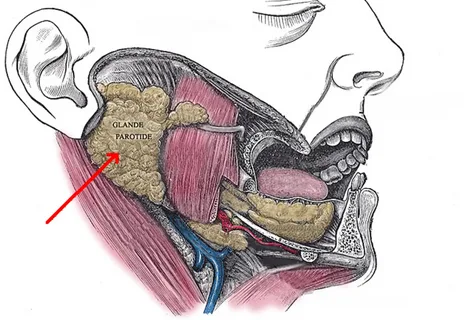
Figure 5. Location of the salivary glands.
Next, the cassette is changed again, and 2 minutes after the catheter is removed, a third image is taken. This corresponds to the phase of resorption and emptying. The last image allows for the assessment of the functional capabilities of the gland; normally, the water-soluble contrast agent is excreted by the gland during this time interval.
More details on the diagnosis of various diseases of the maxillofacial area can be found in the section of our website Training in Maxillofacial Surgery.
