Surgical Stage of Implantation
Machine translation
Original article is written in RU language (link to read it) .
Based on the conducted clinical and laboratory studies, a plan for the surgical and then orthopedic stages of implantation is developed with the participation of the implant surgeon, orthopedist, and dental technician.
What factors need to be considered when choosing the method of immediate implantation in the webinar Immediate Implantation: Secrets of Success.
Tasks that need to be solved at the surgical stage:
- perform implantation according to the planned schedule;
- install the planned number of implants at the designated points;
- ensure conditions that guarantee active reparative regeneration of bone tissue around the implant;
- create conditions for adequate healing of the gingival cuff around the implant;
- clarify the further treatment plan, plan the period of functional integration of the implant, based on the analysis of the architecture of the bone tissue and the position of the implants relative to the compact layer.

Figure 1. Dental implantation in complete edentulism.
The surgical stage consists of the following manipulations:
- preoperative preparation;
- the actual surgical intervention;
- postoperative observation.
Dental implantation is an outpatient surgical intervention performed under local anesthesia. The fundamental principle of dental implantation is the atraumatic nature of the intervention. Implantation is carried out with strict adherence to the principles of asepsis and antisepsis in an operating room equipped with all necessary equipment and instruments that meet the dental profile.
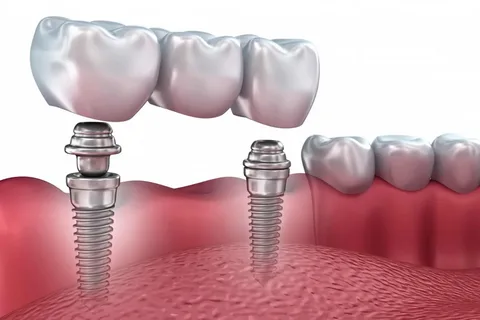
Figure 2. Implantation in case of terminal defect.
In addition to the main equipment required for implantation, additional equipment will be needed – a piezoelectric dispenser (a device that allows for bone preparation). The design of the piezoelectric dispenser provides the supply of a cooling solution, which is important during bone preparation, and the tips included in the device are equipped with a reducing gear, which ensures gentle drilling of the bone tissue.
For dental implantation, a vacuum suction device and a set of implantation tools will also be required.
Preoperative Preparation
Preoperative preparation involves the preparation directly for dental implantation, during which comprehensive oral cavity sanitation is carried out with the participation of a therapist dentist, a dental surgeon, and a prosthodontist.

Figure 3. Professional hygiene.
Activities that need to be performed at the preoperative preparation stage:
removal of severely damaged teeth, teeth with high mobility that cannot be subjected to conservative treatment;
- performing professional hygiene (removal of supragingival and subgingival deposits);
- treatment of caries and its complications;
- training the patient in adequate care for prostheses, maintaining a high level of personal hygiene;
- if necessary, a course of periodontal treatment is recommended to eliminate inflammatory processes in the periodontal tissues.
It is important to allow for a waiting period to enable the bone tissue in the area of the extracted teeth to recover, during which the manufacture of temporary prostheses is planned.
Thanks to modern advancements, it has become possible to perform surgeries to increase the volume of bone mass against the backdrop of atrophy of the alveolar ridge. Autogenous bone or synthetic substitutes (guided tissue regeneration technique) may be used for this purpose.
At this stage, bone plastic surgery is indicated to increase the height of the bone mass of the alveolar ridge (usually in the lateral areas of the upper jaw) or to increase the width on the vestibular surface (this primarily concerns the frontal section). Bone plastic surgery is performed based on strictly justified indications.
Regardless of the volume of the proposed interventions, the patient during the consultation or in the process of preliminary examination should clearly understand all possible options for restoring the dental arch, and be familiar with the advantages and risks of dental implantation.
Dental Implantation Techniques
Dental implantation can be carried out in one or several stages; these are standard basic interventions.
Two-Stage Technique
- In the first stage, the installation of the endosseous element is performed.
- The second stage of the surgical intervention on the upper jaw is performed after about 6 months, on the lower jaw a little earlier – after 3-4 months. It involves incising the mucous membrane over the endosseous element, extracting the cover screw, preparing the abutment, the gingival former, and other orthopedic components that are part of the implant structure.
One-Stage Technique
This technique is used in situations where the implantation of non-removable models of implants (screw, plate) is planned into the jawbone.
Plate implants used in the clinic as a support for subsequent prosthetics have shown excellent long-term results, but it is important to strictly adhere to the indications for their use and correctly select the orthopedic structure.

Figure 4. Immediate implantation after tooth extraction.
Indications for the use of plate implants
- unilateral and bilateral terminal defects;
- included defects of significant length within the dental arch;
- significant atrophy of the alveolar ridge (thickness from 3 mm);
- re-implantation.
Positive qualities of plate constructions
- relative simplicity of execution;
- low cost compared to other models;
- possibility of installation on a narrow alveolar ridge;
- relatively short prosthetic period (under favorable conditions, it takes no more than a few weeks).
Disadvantages of plate constructions
- the bed is formed incongruently;
- the prosthesis includes at least two natural teeth;
- implants communicate with the oral cavity.
Sequence of installation of plate constructions:
- a cut is made along the alveolar ridge;
- the mucoperiosteal flap is detached;
- marking for the implant bed length is performed;
- using special fissure burs, the bone bed is gradually formed;
- the direction and size of the bed are checked with an implant analog;
- the implant is inserted into the bed, with the shoulders and necks being submerged tightly;
- the edges of the mucoperiosteal flap are adapted relative to the implant head;
- stitches are applied, and the wound is sutured.
Non-removable implants, the intraosseous part of which has a diameter of 2.8-3.0 mm, are also installed in a single stage. Suture removal is performed on the 7th-8th day.
Today, many specialists prefer the two-stage technique for installing screw structures, as it promotes better osseointegration and ensures the long-term functioning of the finished structure. The two-stage method also has a lower risk of complications.
Indications for cylindrical and screw implants
- terminal defects;
- included defects;
- complete edentulism;
- absence of individual teeth;
- bone volume from 5 mm.
Stages of surgical intervention:
- incision and detachment of the mucoperiosteal flap along the crest of the alveolar process;
- the crest is corrected with a surgical drill;
- the bone bed is formed using special drills, with a rotation speed of 600-800 revolutions per minute, and the diameter increases sequentially to the diameter corresponding to the implant to be installed;
- the intraosseous element of the screw implant is placed in the bed 1.0-1.5 mm below the level of the alveolar crest;
- a cover screw is necessary to prevent the mucosa from growing into the internal channel of the implant;
- the mucoperiosteal flap is placed back and sutured.
If there is a bone deficiency, the volume is compensated through bone-plastic surgeries.

Figure 5. Bone-plastic surgery.
Advantages of the two-stage technique
- the implant has a tight contact with the bone tissue, ensuring reliable primary fixation;
- there is no communication with the oral cavity;
- there is no need to prepare adjacent teeth;
- good aesthetic and functional result of prosthetics.
Immediate Implantation
The indications for it have been expanded recently. The technique involves the placement of an implant directly into the socket immediately after tooth extraction.
The main condition is sufficient bone mass in the socket. When placing the implant in the socket, it is precisely positioned along the axis of the tooth, relative to the neighboring teeth, which ensures an optimal distant aesthetic and functional result, significantly reducing the rehabilitation period.
On the effectiveness of immediate implantation in the webinar Immediate Simultaneous Implantation.
