Costen's Syndrome
Machine translation
Original article is written in RU language (link to read it) .
Diseases of the temporomandibular joint are a set of pathological processes that affect all structural components of the joint itself, as well as the masticatory muscles, accompanied by impairment of the normal functioning of the lower jaw and the appearance of pain syndrome in the jaw and facial area.
More on this topic in the online course TMJ Dysfunction: A Modern Perspective on the Problem.
Diseases of the temporomandibular joint often become the cause of the suppression of vital functions of the body: breathing, speech, nutrition, as well as psycho-emotional disorders, which as they progress lead to the patient's disability and worsen their social status.
Principles of Diagnosis
The basis of the diagnosis of temporomandibular joint diseases lies in the careful collection and analysis of clinical data, conducting functional and radiological studies.
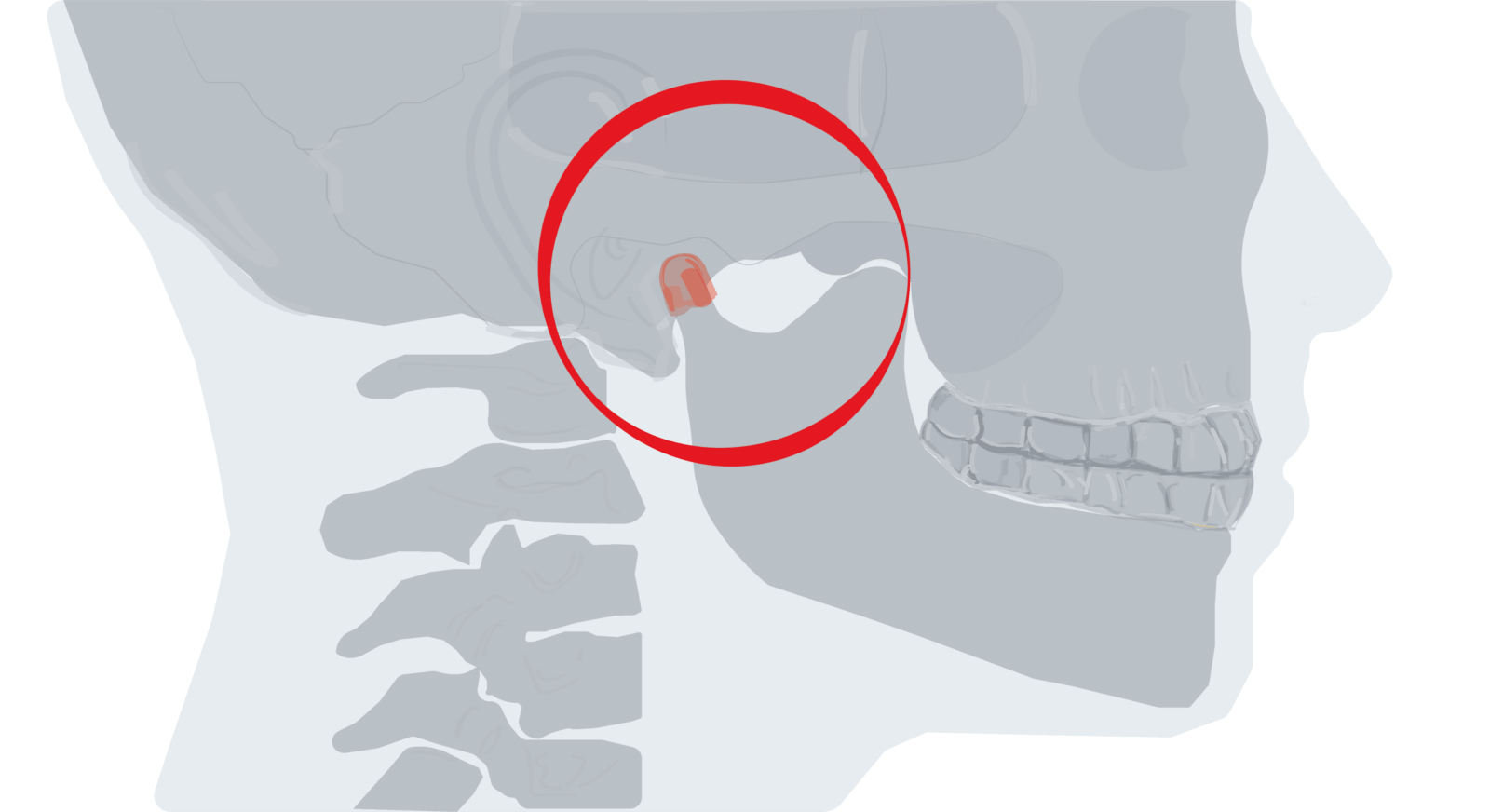
Figure 1. Localization of pain in Costens syndrome.
Among the physical examination methods, the collection of patient complaints and medical history is of key importance. The following clinical procedures should be highlighted:
- visual examination of the dental and jaw system;
- external assessment of the temporomandibular joint;
- auscultation and palpation of the joint;
- assessment of joint mobility;
- palpation of the masticatory muscles, as well as the muscles of the neck and upper limb girdle.
Among the diverse radiological examination methods for temporomandibular joint pathology, the following have gained the most value:
- tomography,
- panoramic zonography,
- orthopantomography,
- computed tomography,
- magnetic resonance imaging,
- volumetric dental tomography.
Magnetic resonance imaging is the gold standard for diagnosing damage to the soft tissue structures of the temporomandibular joint. This is due to the fact that, unlike other radiological methods, MRI visualizes the articular disc and surrounding ligamentous apparatus, as well as the joint capsule under conditions of natural contrast.
Among the functional diagnostic procedures, the following have significant practical importance:
- electromyography of the masticatory muscles,
- axiography,
- audiography of the sound phenomena of the joint,
- MPI – analysis (assessment of jaw position).
As modern technologies develop and are integrated into dental practice, endoscopic technologies are gaining increasing popularity in the diagnosis of pathological conditions of the joint.
The nature of temporomandibular joint diseases is polyetiological. Among the causes that lead to the formation of pathological changes in the joint, many local and systemic factors can be identified.
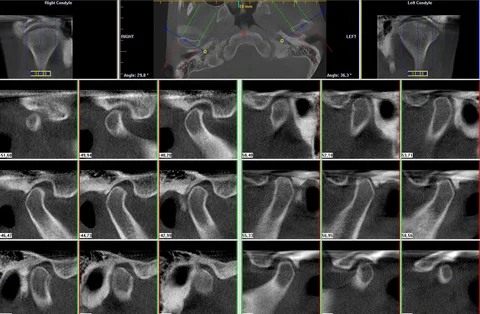
Figure 2. Joint tomography.
Scientists have proven that in the process of developing initial symptoms of functional disorders, which subsequently lead to the emergence of structural changes in bone and soft tissue formations, the following factors have a direct influence:
- the presence of occlusion disorders,
- the condition of the musculoskeletal system and muscle apparatus, including the spine,
- the condition of the internal structures of the joint,
- the psycho-emotional status of the patient.
This article will focus in more detail on one of the pain dysfunction syndromes of the TMJ (TMJ pain dysfunction syndrome), the Costens syndrome.
Costens Syndrome
According to the ICD-10 classification, this pathological condition has the code K07.60.
Diagnosis of Costens Syndrome
This disease occurs with equal frequency among adult patients and children.
The pain dysfunction syndrome is characterized by chronic pain that is localized around the joint itself, as well as in the masticatory muscles, and is typically radiating along the lower jaw, to the ear, teeth, head, and neck.
It is common to distinguish two main etiological factors of pain that occurs in the projection of the joint. This pain syndrome can be caused by muscle spasm; in this case, the pain has a myogenic nature. The second, arthrogenic nature, originates from the soft tissue structures of the joint, which are injured due to changes in the natural position of the mandibular head.

Figure 3. The condylar process of the mandible.
Myogenic pain is predominantly associated with a history of muscle injury; this can be a result of sudden overstrain when biting hard food, a consequence of the development of myositis, or psycho-emotional stress.
Arthrogenic pain is a consequence of overstretching the intra-articular ligaments of the joint, localized in the joint capsule, or is the result of compression of the bilaminar zone in the case of posterior displacement of the articular head (compression syndrome), which mimics the clinical presentation of ear disease.
Main clinical manifestations of TMJ dysfunction
- Spontaneous pain, often trigger points are identified in the masticatory muscles or neck muscles.
- Radiation of pain may be observed in different parts of the body, head, neck, teeth, jaws, palate, ear, eye socket, throat.
- A precursor to pain often is pathological mobility of the jaw, clicking in the joint.
- Characteristic are periodic and constant hearing disturbances, dull pain in the ear area, tinnitus, headache, eye pain, dizziness.
When collecting the medical history, it is important to remember that the Costens syndrome or pain dysfunction of the joint has a polyetiological nature, but even among this diversity, several key factors can be highlighted that directly influence the development of the disease symptoms:
- the condition of the spine and muscular system,
- the presence of occlusion disorders,
- the internal condition of the joint structures,
- the psycho-emotional status of the patient.

Figure 4. Pain irradiation in the case of TMJ pain syndrome.
During the clinical examination, the condition of the temporomandibular joint is visually assessed, the masticatory muscles and the joint are palpated. Often, during palpation, trigger points are identified in the muscle tissue, signs of referred pain are revealed, and factors that provoke the onset of pain are identified. The latter include the following:
- occlusal instability,
- presence of parafunctions,
- bad habits.
It is important to thoroughly assess the dental status of the patient during the initial visit (defects in the dental arches, deformations, inadequate prostheses or fillings, elevated bite, disturbances in the interalveolar distance). Among systemic factors, identifying pathologies related to the musculoskeletal system and spine, as well as assessing the psycho-emotional status of the patient, is of primary importance. It is necessary to palpate the muscles of the neck and the shoulder girdle.
Differential Diagnosis
Kosten's syndrome should be differentiated from infectious, traumatic, and inflammatory arthropathies. Other diseases that require differential diagnosis of TMJ disorders include:
- arthritis of various etiologies,
- migraine,
- neuralgias of various nerves: glossopharyngeal, branches of the trigeminal, tympanic nerves, neuralgia of the pterygopalatine ganglion,
- temporal arteritis,
- styloid process syndrome,
- cervical osteochondrosis.
The collection of the disease history and a thorough clinical examination of the patient contribute to the differential diagnosis.
For instance, purulent arthritis is accompanied by swelling of the soft tissues near the affected joint, pain in the area of inflammation. Upon palpation of the joint, acute pain occurs, and limitation of mouth opening is characteristic.
Rheumatoid arthritis is a systemic chronic connective tissue disorder, against which the joints become involved in the pathological process, and the clinical picture resembles destructive arthritis.
A set of signs typical for rheumatoid arthritis:
- at the time of examination and in the history, pain is localized in several different joints simultaneously;
- symmetry of joint involvement;
- swelling, limited mobility in several joints, rapid involvement of the hands, feet, wrists;
- positive test for rheumatoid factor.
If at least two of the above criteria are identified in the patient, a diagnosis of rheumatoid arthritis can be confidently made.
In case of suspicion of psoriatic arthritis, in addition to inflammatory signs in the joint, attention should be paid to psoriatic changes in the skin and nails, as this is the main diagnostic sign of the disease.
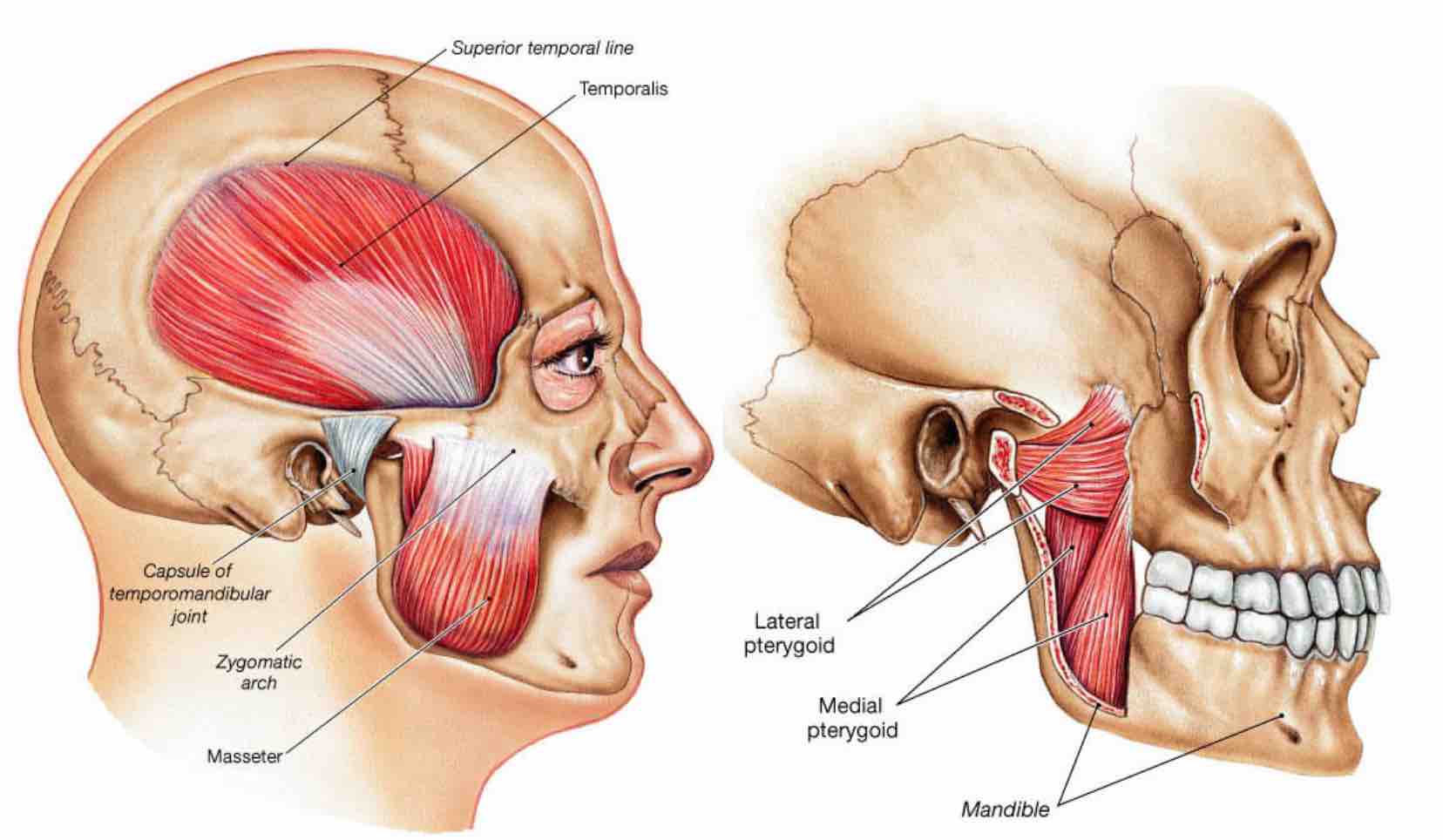
Figure 5. Masticatory muscles.
To conduct a differential diagnosis of Costen's syndrome with neuralgias, it is important to remember that the latter is characterized by the presence of trigger zones, after irritation of which the patient experiences a sharp attack of pain.
Treatment Principles
Treatment of this condition involves the collaboration of many specialists, starting from the maxillofacial surgeon, orthopedic dentist, and orthodontist, to the physiotherapist, orthopedic traumatologist, psychiatrist, and psychotherapist. The goal of treatment is to eliminate pain, normalize the anatomical structures of the TMJ, and the function of the masticatory muscles, as well as to prevent recurrences.
Principles of neuromuscular dentistry in the webinar Treatment of muscle-joint dysfunctions and cranio-cervical-mandibular dysfunctions in the concept of neuromuscular orthodontics.
