Odontogenic Sinusitis: Clinic and Differential Diagnosis
Machine translation
Original article is written in RU language (link to read it) .
The size of the maxillary sinus at birth is less than 10 mm in any direction. By the age of 12-14 years, the floor of the sinus is located at the level of the floor of the nasal cavity. The end of the sinus growth corresponds to the moment when all permanent teeth erupt. The maxillary sinus communicates with the nasal cavity through an opening in the middle nasal meatus.
The principles of treatment for patients with diseases of the maxillary sinus are discussed in the online course Pathologies of the Maxillary Sinus: The Role of the ENT Doctor and Dentist.
Features of Anatomical Structure
The maxillary sinus is the largest of all paranasal sinuses. Its configuration resembles a quadrangular pyramid:
- the floor of the orbit is the upper wall,
- the base of the alveolar process is the lower wall,
- the lateral surface of the nose is the medial wall,
- the zygomatic process of the jaw from its tuberosity is the lateral wall,
- the alveolar process and body of the jaw form the anterior wall, which also serves as the walls of the pterygopalatine and infratemporal fossae.
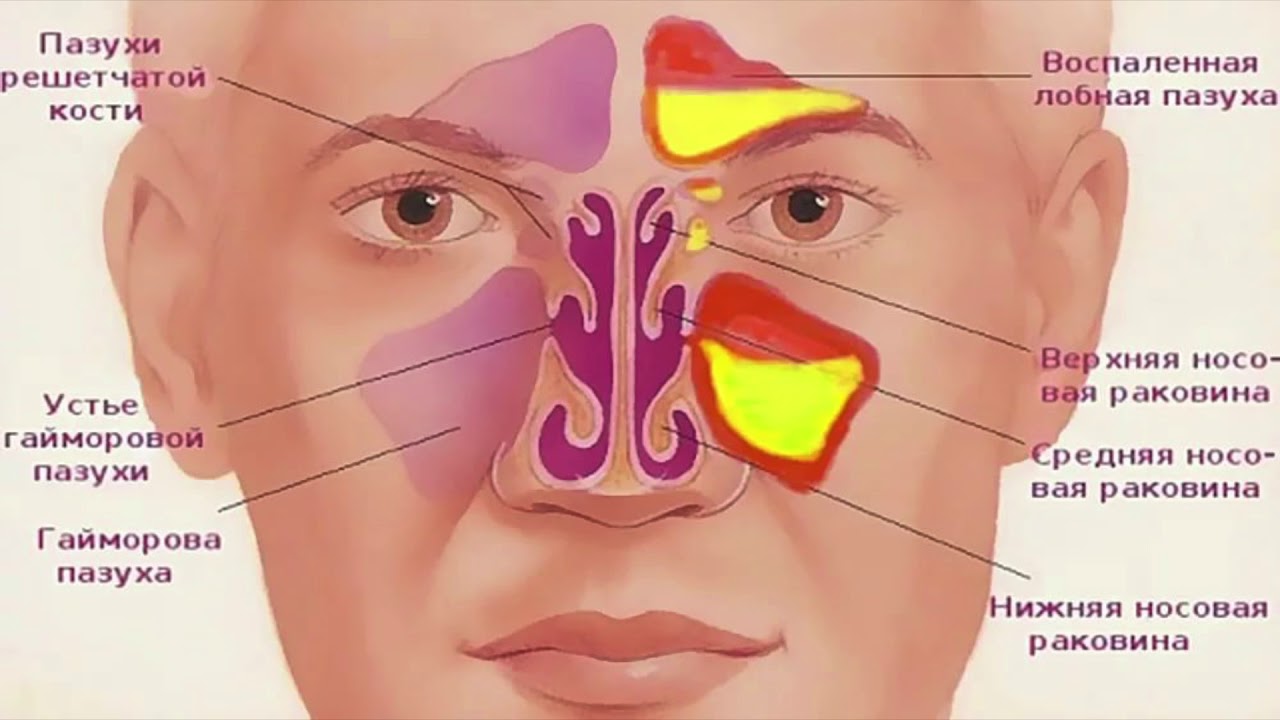
Figure 1. Accessory sinuses.
The volume of the sinus in an adult is on average 15 cm3. The mucosa of the maxillary sinus is a continuation of the nasal mucosa, which grows from the nose through natural openings. It is lined with ciliated pseudostratified epithelium with a loose connective tissue base that is richly supplied with blood.
Classification of Sinusitis
Based on their origin, sinusitis can be divided into the following types:
- rinogenic;
- odontogenic;
- traumatic;
- hematogenic.
Odontogenic Sinusitis
Odontogenic inflammation is an inflammatory process that arises in the maxillary sinus due to the penetration of toxins or infection from an odontogenic focus.
The following causes of inflammation and sources of infection of the maxillary sinus are identified:
- foci of inflammation in the area of the apices of the first molars and second upper premolars, less often other molars;
- periodontal diseases;
- osteomyelitis of the jaw;
- mechanical pushing of decay from the canal into the sinus;
- periradicular cysts;
- pushing fragments of endodontic instruments;
- careless manipulations after tooth extraction when scraping granulomas during the revision of the socket.
The pathological process, which has existed for a long time in the periodontium or in the periapical tissues of the upper teeth, the roots of which are adjacent to the bottom of the sinus, does not immediately contribute to the development of sinusitis, although infection of the sinus undoubtedly occurs as a result of contact or dissemination of infection through lymphatic capillaries. Frequent exacerbations of the pathological process in periapical foci adjacent to the sinus provoke changes in its mucosa, preparing it for the development of inflammation.
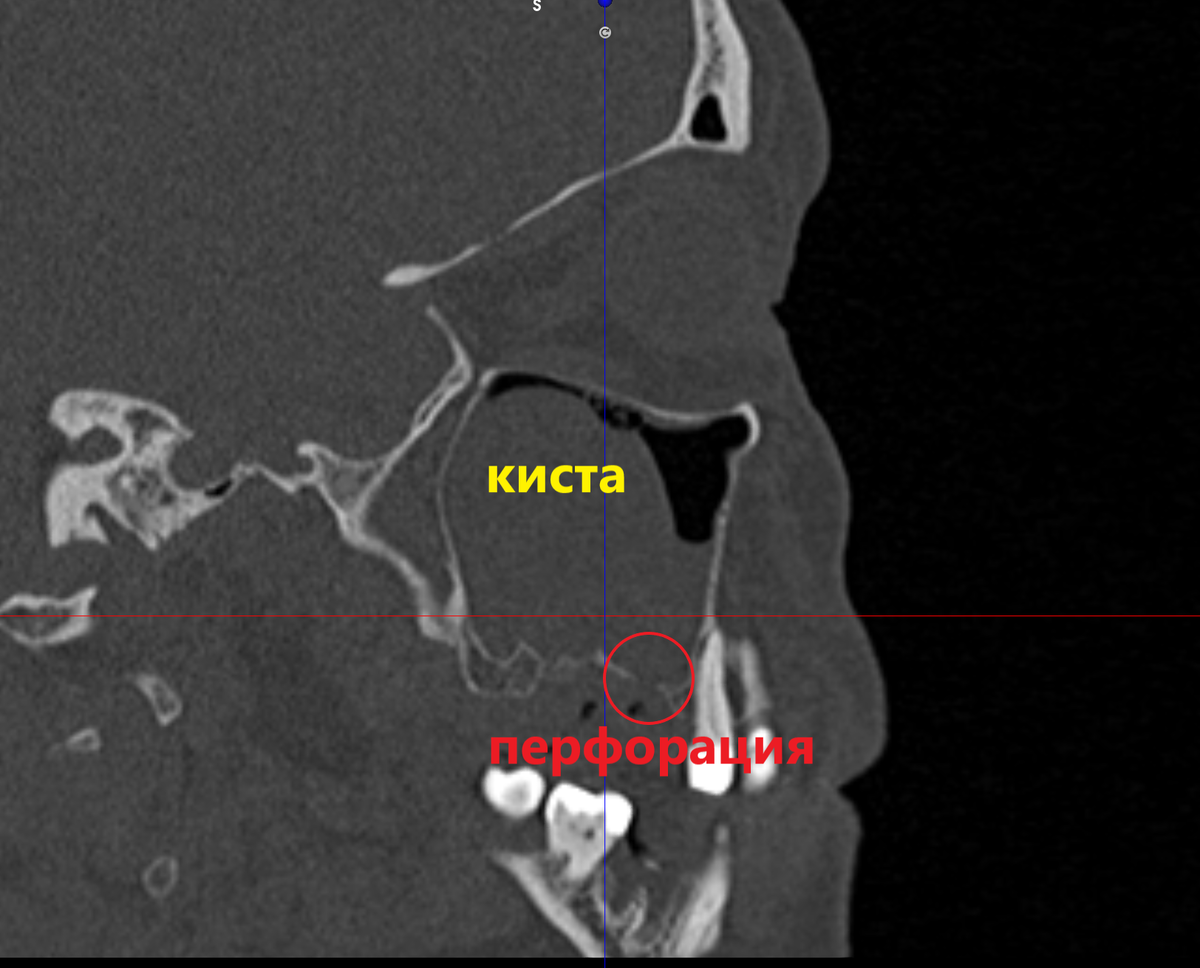
Figure 2. Perforation of the maxillary sinus.
Macroscopically, swelling, edema, and thickening of the sinus mucosa are observed. Microscopic changes: abundant polymorphonuclear infiltration, desquamation of the epithelium, which progressively leads to the formation of erosions.
Odontogenic Sinusitis. Classification
All odontogenic sinusitis can be divided into acute forms, which in turn are divided into:
- catarrhal,
- serous,
- hemorrhagic,
- fibrinous-purulent.
Also chronic forms:
- parietal-hyperplastic,
- polypous.
The type of inflammatory reaction depends on the nature of the exudate. If the cause of inflammation is bacteria, and odontogenic sinusitis most often has a bacterial nature, the process proceeds with the formation of pus. In the case of a viral nature, the inflammation is catarrhal, serous, or hemorrhagic.
Clinical Picture of Acute Odontogenic Sinusitis
Initially, the disease is accompanied by a feeling of tension and pressure in the area of the inflamed sinus, with nasal congestion on one side. Patients complain of pain and heaviness in the area of the affected maxilla, which intensifies when tilting the head down, a deterioration in smell, and the appearance of mucus from the nostril on the side of the inflammation.
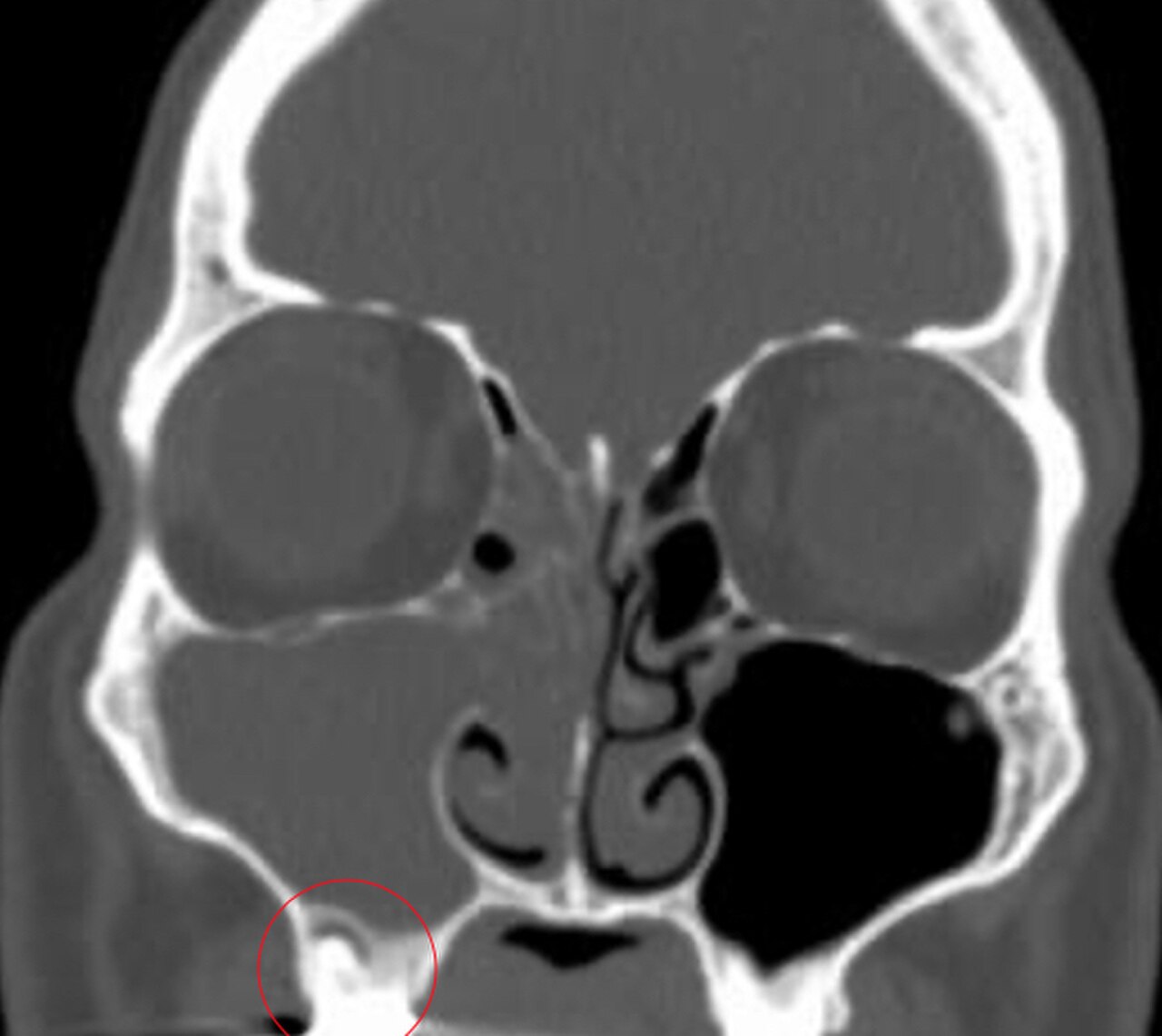
Figure 3. Radiological signs of sinusitis.
The intensity of pain increases with the development of inflammatory phenomena. Pain radiation is observed in the eye, temple, forehead, and upper teeth. Mucus is discharged from the nasal cavity on the affected side, and the process intensifies when the head is tilted; sense of smell is lost.
The general condition of the patient is suffering:
- temperature rises,
- headache occurs,
- fatigue,
- weakness,
- lack of sleep.
External examination reveals swelling of the lower eyelid and cheek, palpation of the fossa Canina is painful. There is an odontogenic source in the mouth that has provoked the development of inflammation of the maxillary sinus. Percussion of the upper teeth (molars) on the side of the inflammation causes pain. Locally, hyperemia and edema of the mucosa (mainly of the inferior nasal concha) are found, and purulent discharge is present in the middle nasal meatus. To confirm the presence of pus, it is recommended to perform puncture and aspiration using a syringe. Radiological examination shows varying degrees of opacity in the maxillary sinus.
Chronic odontogenic sinusitis
A common cause of development is the result of an untreated acute process; however, the disease can be primarily chronic without preceding acute manifestations, due to infiltration of the sinus from the odontogenic focus by microflora during perforation of the sinus floor during the extraction of upper teeth.
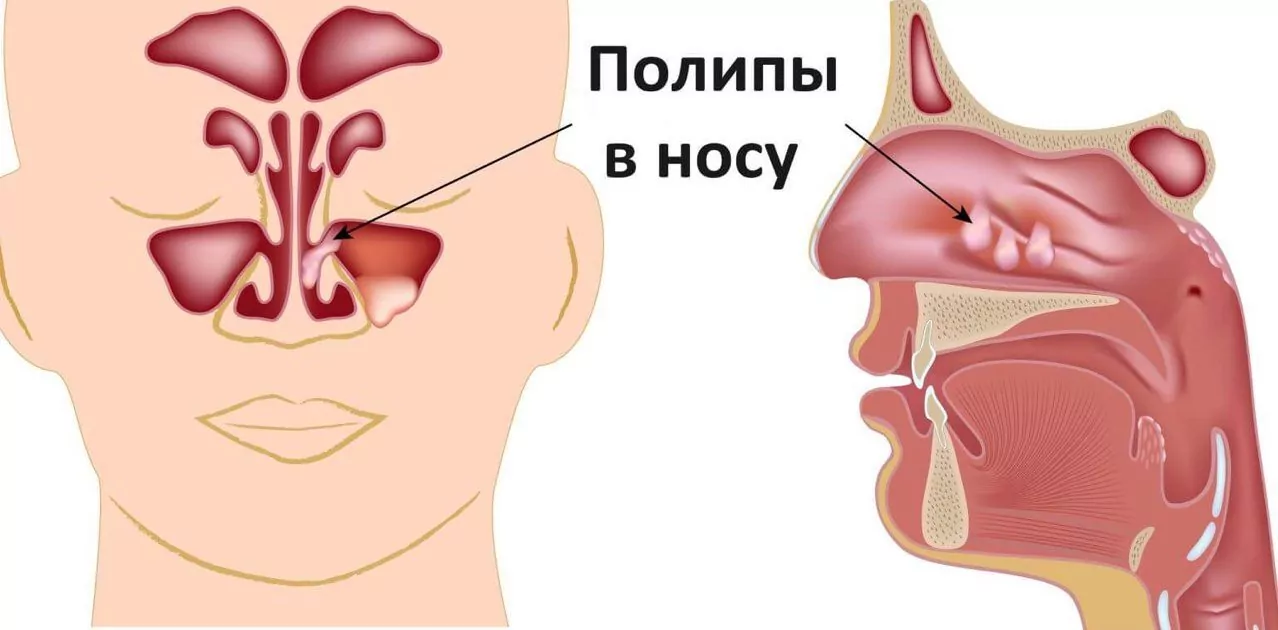
Figure 4. Polypous form.
Mucosal changes are determined by the degree of damage and the nature of the pathological process. Swelling and thickening of certain areas of the mucosa on the lower surface of the sinus may be observed, or granulations or protrusions of the mucosa with a broad base may form, which is characteristic of the polypous form. Purulent or mucus-containing discharge is noted.
Microscopically, signs of productive reactions prevail. The epithelial layer thickens sharply. Erosions, and sometimes even ulcers, form on the surface of the epithelium.
Typical symptoms:
- pus from one side of the nose,
- discharges are often foul-smelling,
- nasal breathing is difficult,
- headache is predominantly unilateral,
- heaviness in the head,
- radiation of pain along the branches of the trigeminal nerve.
X-ray signs:
- Decreased transparency of the sinus; against the background of pus accumulation, the picture becomes more intense and homogeneous.
- Wall "veil," as well as shadows of various sizes, are determined in the polypous form.
Contrast radiography has high informative value, allowing for clarification of the diagnosis, determination of the location, and extent of the pathological focus.
Odontogenic sinusitis. Differential diagnosis
Distinctive features of odontogenic sinusitis from rhinogenic:
- unilateral inflammation, in the case of rhino-genic process – bilateral;
- lesion of the mucosa only in the area of the bottom (in the case of rhino-genic inflammation, the entire mucosa is involved);
- toothache precedes the disease, there is an odontogenic focus.
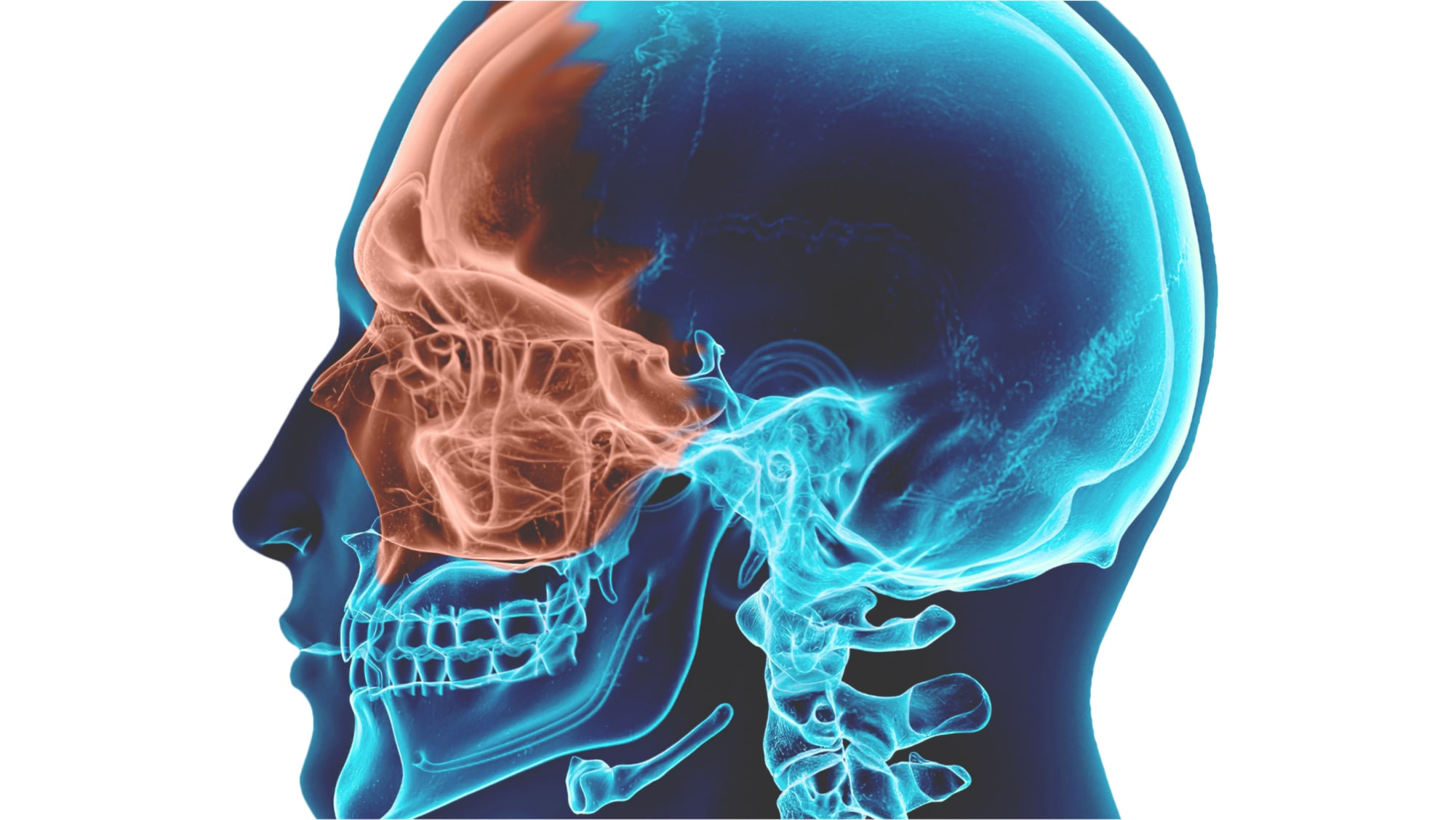
Figure 5. Area of research in case of suspected sinusitis.
Differences from allergic sinusitis:
- absence of an odontogenic source in allergic inflammation;
- longer course of allergic sinusitis with remissions and exacerbations;
- inflammation of allergic origin spreads to the mucosa of the nose and other sinuses.
Differential diagnosis with periodontitis:
- absence of nasal congestion, feeling of heaviness;
- absence of nasal discharge;
- tooth destroyed by caries in the oral cavity;
- X-ray changes in the sinus are absent, but present in the area of the tooth apex.
With neuralgia:
- pain is paroxysmal, spontaneous,
- tendency for periodicity of attacks;
- "trigger" zones;
- no nasal discharge, sense of smell is not impaired;
- X-ray signs of inflammation are absent;
- temperature does not rise.
Differential diagnosis of chronic odontogenic sinusitis
Differences from periapical cysts:
- bulging and deformation of the alveolar process of the jaw or canine fossa;
- dome-shaped outline of the boundary of transparency change on the X-ray.
Distinctive features of odontogenic sinusitis in chronic form from malignant tumors:
- pain in the neoplasm is more persistent, constantly increasing;
- nasal discharge has a blood admixture;
- anti-inflammatory therapy is ineffective;
- characteristic displacement of the eyeball, deformation of the sinus;
- tumor-like growths are found in the socket after tooth extraction, in the nose.
Treatment
Treatment involves eliminating the odontogenic focus of inflammation, establishing drainage of the sinus for several weeks. The sinus is rinsed with antiseptic solutions.
Surgical treatment is indicated in the presence of parietal hyperplastic growth of the sinus mucosa, in the polypoid form, ineffectiveness of conservative treatment, infiltration of cysts into the sinus or pushing foreign bodies into it.
Classification, etiology, clinical picture, diagnosis, and treatment of maxillary sinusitis are described in detail in the webinar Treatment of Maxillary Sinus Pathologies for Successful Sinus Lifting.
