Temporomandibular Joint Dysfunction: Etiology and Pathogenesis
Machine translation
Original article is written in RU language (link to read it) .
Temporomandibular joint dysfunction is a pathological condition that is accompanied by a disruption of its normal functioning, characterized by changes in the direction and volume of movement of the lower jaw, as well as a whole complex of other symptoms:
- pain syndrome;
- auditory phenomena during jaw movement;
- headaches;
- chewing function impairment;
- sensation of ear fullness.
More details on this topic in the online course Temporomandibular Joint Dysfunction: A Modern Perspective on the Problem.
Etiology of TMJ Dysfunction
The most common causes that can lead to TMJ dysfunction:
- malocclusion, not only congenital but also related to prosthetic errors;
- damage to the masticatory muscles, dystonia;
- disorders related to the pathological position of the intra-articular disc and its displacement;
- pathology of the ligamentous apparatus that fixes the disc to the joint capsule and the condyle.
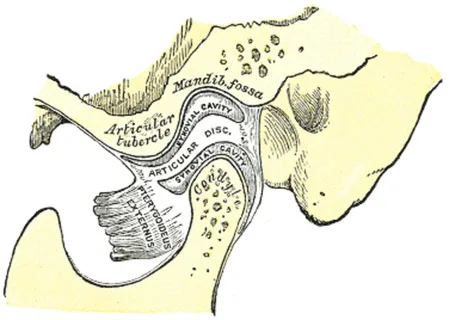
Figure 1. Structure of the temporomandibular joint.
TMJ dysfunction has typical clinical manifestations associated with impaired excursion of the lower jaw, characterized by the following symptoms:
- mouth opening is limited;
- when opening the mouth, the lower jaw shifts to one side;
- mouth closing is limited.
The most common complaints that a patient may present are as follows:
- pain sensations;
- noisy phenomena in the joints;
- sensation of ear congestion;
- difficulties in biting and chewing during meals;
- sensation of tightness and fatigue in the masticatory muscles;
- shifting of the lower jaw to one side.
If we take each of the above symptoms individually, it occurs in 35% of patients, but various combinations of these symptoms are characteristic of 65% of patients.
TMJ Dysfunction. Pathogenesis of Pain
The pain in some patients with TMJ dysfunction is myogenic in nature, and it is most often associated with the following factors:
- trauma or suddenly occurring muscle strain at the moment of biting hard food;
- myositis;
- psycho-emotional excitement.
The source of pain in another group of patients is intra-articular disorders, among which the following can be highlighted:
- the head or intra-articular disc shifts backward, causing injury to the plexus located in the bilaminar area (the distal part of the disc is firmly connected to strong connective tissue fibers, which are attached around the perimeter of the joint cavity by the bilaminar zone, where a developed vascular-nerve plexus is located);
- tears of intra-articular ligaments.
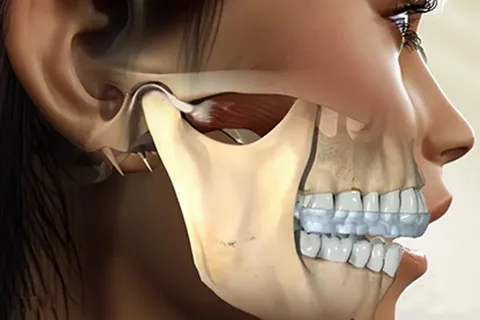
Figure 2. Temporomandibular joint.
Intra-articular disorders cause joint pain, the nature of which is called arthrogenic. However, a significant part of the pain syndrome may be attributed to the muscular component, more specifically – excessive stretching of the lateral pterygoid muscle.
But even in the case of hypertonicity of the lateral pterygoid muscle, pain is often predominantly caused by other factors, namely:
- excessive stretching of the intra-articular ligaments;
- tension of the joint capsule;
- compression of the bilaminar area.
The greatest difficulties arise in situations where the pain syndrome in the area of the TMJ is caused by a combination of several factors: hypertonicity and pain of the lateral pterygoid muscle, related to the correction of occlusal relationships through prosthetics.
To summarize all of the above, the pain syndrome in the area of the TMJ develops as a result of:
- excessive pressure on the vascular-nervous plexus of the bilaminar zone;
- atypical direction and strength of stretching of the capsule and ligaments of the joint;
- irritation of the vascular-nervous endings in the muscles surrounding the joint, or their hypertonicity.
Prerequisites for the onset of the pain syndrome may include:
- bite pathology, especially the removal of lower molars;
- errors at the stage of prosthetics related to the violation of bite height;
- the patient being in an open-mouth position for an extended period during dental treatment;
- recent psycho-emotional stress;
- sudden one-time overstrain of the masticatory muscles during wide mouth opening;
- chronic stress states;
- correction of occlusal relationships after prolonged complete edentulism;
- presence of partial secondary edentulism for a long period of time.
Pain syndrome is diagnosed in patients who have one of the aforementioned causes, against the background of chronic stress, overstrain of the nervous system, with concomitant thyroid pathology, against the background of gynecological diseases. The overwhelming majority of patients with TMJ dysfunction are women.

Figure 3. Lower jaw and condylar process.
The nature of the pain in TMJ dysfunction among patients and its irradiation is quite diverse; it can be very difficult to determine the nature of the pain. In cases where the pain sensations in the TMJ area are related to the pressure of the head of the lower jaw on the bilaminar zone or overloads of the ligamentous apparatus of the joint, the localization of pain is in the TMJ area, irradiation occurs in the ear, and pain sensations are intensified during jaw movement.
Clinical Symptoms
- moderate tenderness upon palpation of the lateral pterygoid muscle, increased pain with muscle tone elevation;
- localization of pain in the joint area when applying vertical load to the angle of the mandible;
- reduced range of motion of the articular head on the affected side;
- mouth opening is limited.
Radiological Symptoms
- upon mouth opening, the articular head shifts backward beyond the space of the glenoid fissure, which is associated with the anterior displacement of the intra-articular disc;
- the range of motion of the articular head is minimal.
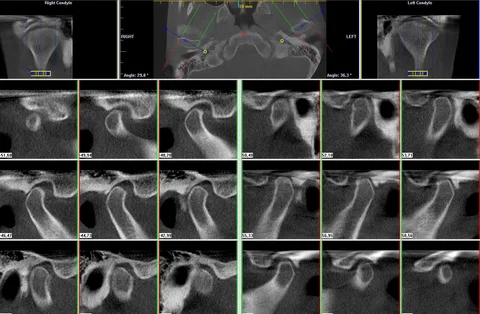
Figure 4. CT of the TMJ.
The combination of clinical and radiological symptoms is referred to as a "block" of the joint, which will later cause anterior displacement of the disc. Normalization of the disc position in such patients will lead to a reduction in pain syndrome or a change in the nature of the pain, and will increase the range of jaw movements.
Pathogenesis of noise in TMJ dysfunction
"Noisy phenomena" are a cardinal symptom of TMJ dysfunction; they manifest as cracking, crepitation, and friction, and are predominantly diagnosed among patients with intra-articular relationship pathology that causes folding or displacement of the disc, which occurs due to ligament condition disturbances, their tension, and partial mineralization. This pathological process is accelerated as a result of microtraumatization of the ligaments against the background of TMJ dysfunction, as well as the loss of chewing teeth, which leads to increased load on the joint.
The pathological overload occurring in the joint due to the loss of lateral teeth causes the appearance of cracking when opening the mouth at the beginning of the action, at the end, or at the peak. Histological examination of the disc condition reveals swelling of the fibrous cartilage, disorganization, and may show the presence of perforation holes.
"Noisy" phenomena in TMJ dysfunction can manifest as clicks, which are due to another pathological mechanism – a change in the relative position of the articular head and the disc. Clicking occurs because the thickened area of the disc is located anteriorly or at the level of the articular head at rest, and during mouth opening, the head is forced to overcome this obstacle. When closing the mouth, the articular head again has to jump over the thickened posterior edge of the disc.
Disc deformation is most often caused by the following reasons:
- trauma, acute or chronic trauma;
- removal of molars;
- parafunction of the masticatory muscles;
- lack of balance in muscle activity.
The listed factors over time lead to elongation of the posterior and lateral attachments of the disc, weakening of the ligaments, and migration of the disc. The anterior displacement of the intra-articular disc is initially a temporary phenomenon, but then it becomes permanent. Connective tissue at the sites of ligament attachment is constantly injured, further damaged, and the disc gradually shifts further anteriorly, resulting in its persistent fixation in a displaced state.
Sound phenomena, as an isolated symptom, occur in half of the patients with TMJ dysfunction. However, more often, sound phenomena and pain, the leading symptoms of dysfunction, are combined in patients.

Figure 5. Localization of pain in temporomandibular joint dysfunction.
All pathological conditions of the temporomandibular joint are associated with a disruption of the contractile function of the muscles responsible for the movements of the lower jaw, which is often a consequence of malocclusion, and pathological occlusion causes distortion of proprioceptive impulses from the periodontal tissues, leading to muscle tone disturbances, as well as pathology of the soft tissue structural components of the temporomandibular joint.
Overview of risk factors for temporomandibular joint diseases, diagnostic methods, and treatment protocols in the online course Evidence-based treatment of temporomandibular joint dysfunctions.
