Complications of sinus lift surgery
Machine translation
Original article is written in RU language (link to read it) .
Among the complications most commonly encountered after sinus lift surgery are the following: migration of implants into the maxillary sinus, lack of osteointegration in the area of implant reconstruction, inflammatory processes caused by microbial factors.
Learn more about the treatment of sinus lift complications in the webinar Lateral sinus lift: recommendations for workflow organization and treatment of complications.
As infectious agents, it is primarily important to mention microaerophilic and obligate aerobic microorganisms. The inflammatory process in the initial stage is aseptic, but subsequently, pathogenic flora inevitably joins, inhabiting the oral cavity, periodontal pockets, and dental plaque, and the inflammation becomes septic.
In chronic rhinosinusitis after sinus lifting, the bacterial spectrum is predominantly represented by an association of aerobes– 52%, anaerobes – 48%. The overwhelming majority of odontogenic sinusitis is the result of surgical intervention in the area of the upper jaw, alveolar process, macro or micro perforation of the maxillary sinus during tooth extraction. And only in the remaining 5-10% of cases does the inflammatory process develop against the background of a focus of chronic infection near the sinus.
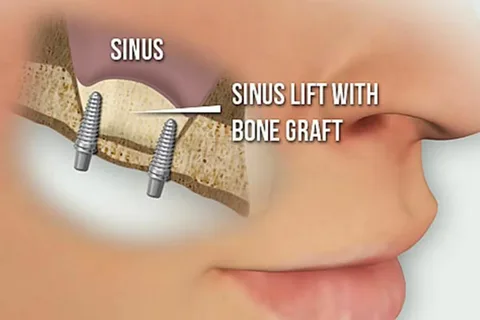
Figure 1. Sinus lift operation.
In recent years, following dental procedures, there has been a significant increase in maxillary sinusitis caused by fungal flora. Mycoses of the nasal sinuses can be caused by fungi from various genera. For instance, Aspergillus fumigatus requires heavy metal salts, which are found in filling materials. Laboratory studies have established that zinc oxide solution positively affects the reproduction of Aspergillus fumigatus, while eugenol (a component of zinc oxide eugenol sealers) suppresses it, but this effect diminishes over time, explaining the formation of sinus mycoses not immediately, but within 2-3 years after the removal of the filling material from the sinus.
In the development of inflammation of the paranasal sinuses, the local pathology of the ciliated epithelium lining the sinus is of great importance, as toxic alteration develops in the area of the filling material, which essentially is a foreign body containing paraformaldehyde, eugenol, and heavy metal salts.
The sensation of pain is also a complication of sinus lifting; it appears several days after the surgical intervention. The pain is caused by osteitis, which develops as a result of overheating of the bone tissue due to insufficient cooling during drilling.
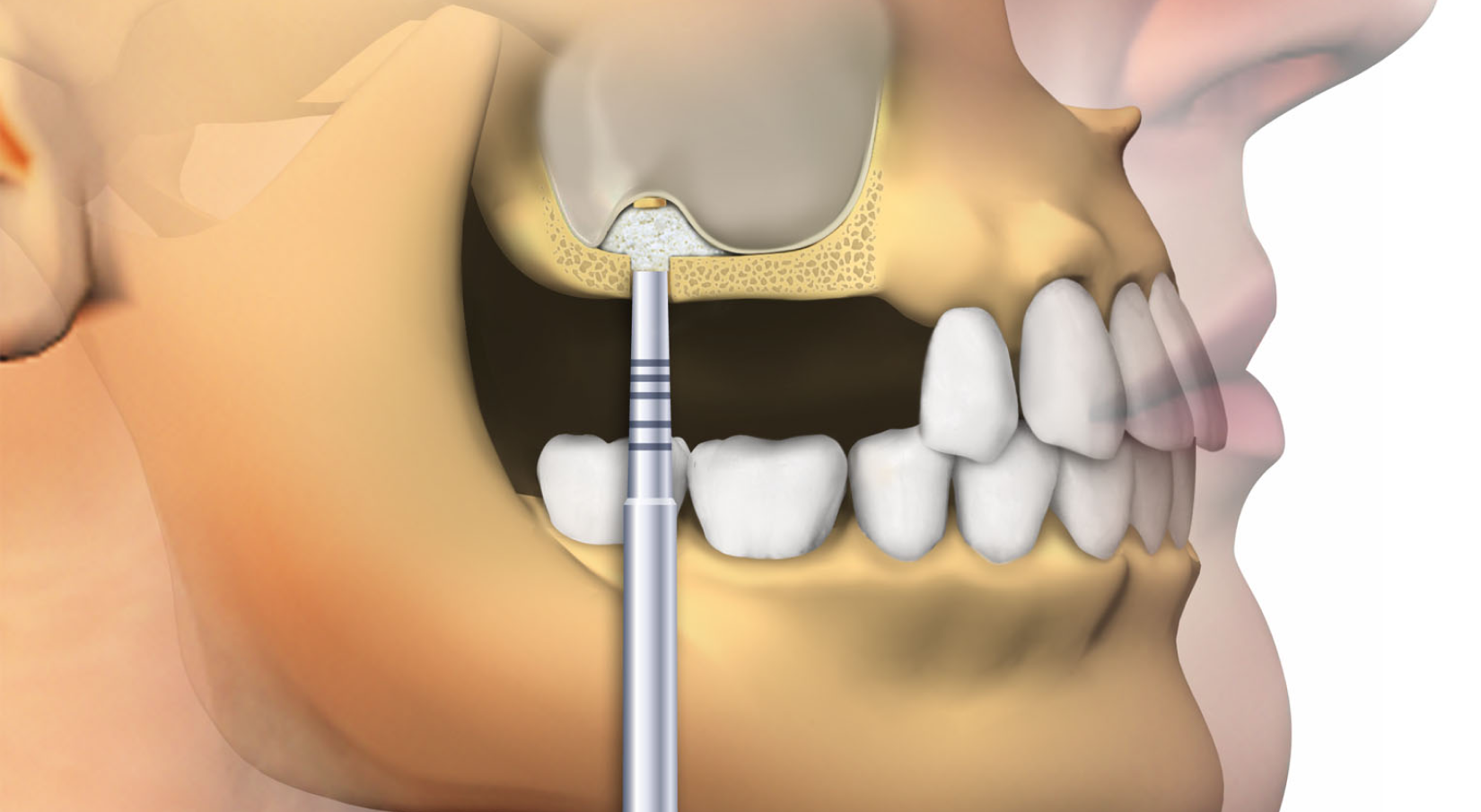
Figure 2. Open sinus lift.
When harvesting a bone block from the chin, the patient may complain of temporary paresthesia or anesthesia in the chin area. These uncomfortable sensations for the patient resolve on their own, without requiring special treatment. Swelling often occurs in the infraorbital area, less frequently - separation of the wound edges. Nasal postoperative bleeding occurs only against the background of perforation of the sinus membrane. The faster the sinus perforation is eliminated, the lower the risk of wound contamination with external pollutants.
Consequences of sinus lift errors
Errors made during the surgical intervention can lead to the following consequences:
- formation of an oroantral fistula,
- appearance of sinusitis symptoms,
- lack of drainage of secretion from the sinus,
- bacterial contamination of the wound,
- development of bleeding.
The most common complication of sinus lifting is rupture of the sinus membrane, which is observed in a third of cases of subantral augmentation.
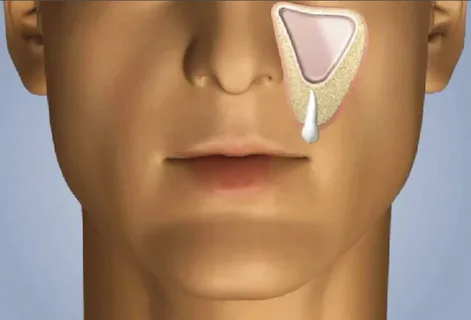
Figure 3. Odontogenic sinusitis.
There are many techniques to close a perforation using various materials. Suturing is the most common procedure.
Materials that can be used to close perforations:
- autogenous bone;
- Bio-Oss;
- resorbable cellulose;
- demineralized freeze-dried laminated bone;
- Collatape, recommended for small defects.
To reduce the risk of perforation during sinus lifting, it is recommended to replace traditional fissure burs and Lindemann burs for osteotomy with spherical diamond burs. Always use adequate cooling with sterile saline during drilling to prevent overheating and burning of the bone tissue.
Partitions inside the sinus create additional complexity during surgery. If they are detected, it is necessary to form separate accesses on both sides of the partition, which will help avoid perforation of the sinus membrane.
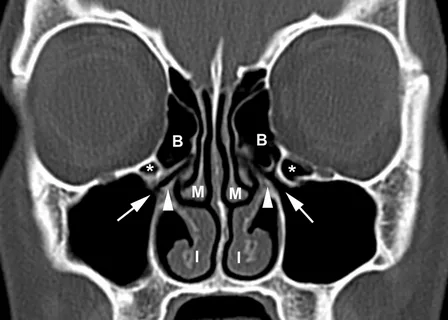
Figure 4. CT scan in sinusitis.
There is a technique that involves peeling the membrane around the perimeter of the entire lower third of the maxillary sinus. In this case, the damaged mucosa ends up on top, the edges of which meet, covering the defect, and later overlapping it. The technique allows covering a small defect, no more than a few millimeters in diameter. After covering, osteogenic material is placed under the mucosa.
During open sinus lifting, fibrin gel, leukocyte or platelet blood fractions can also be used, covering the osteotomy window in the maxillary sinus with a membrane made of these materials.
In case of mucosal perforation, resorbable membranes have proven effective. After localizing the perforation, they are returned to the sinus, covering its inner surface to overlap the boundaries of the lateral osteotomy. Biomaterial is also placed here. The membrane completely covers the biomaterial, preventing it from entering the sinus.
Purulent sinusitis after sinus lifting is often caused by congenital or acquired changes in the architecture of the nasal cavity:
- the presence of polyps in the nasal passages,
- deviation of the nasal septum,
- development of hypertrophy of the nasal conchae.
In some cases, the diagnosis of these pathological conditions during examination or treatment is not carried out, and sometimes it is performed but associated with a number of difficulties. Conventional radiography does not allow for the detection of changes in the ethmoid labyrinth, sphenoid sinus, or nasal cavity, due to the low resolution of radiography and the positioning of the skull bones.
The listed pathological changes facilitate the acceleration of the spread of the inflammatory process from the nasal cavity and paranasal sinuses, create obstacles for sinus drainage, reduce aeration, suppress the functioning of the ciliated epithelium, increasing the likelihood of postoperative complications.
Computed tomography is a method that allows assessing the following parameters:
- the degree of disturbance, its volume and nature, determine the exact localization and detect the thickness of the mucosa;
- establish the density of the mucosa, which is important for assessing the stage of inflammation;
- allows for the diagnosis of the presence of pseudocysts and osteophytes in the mucous membrane of the sinus;
- assesses the presence and nature of the exudate;
- helps detect pathology of the periosteum and bone structures.
This method is necessary to determine the exact signs of disturbances in intranasal structures, lesions of the ethmoid labyrinth, and sphenoid sinuses.
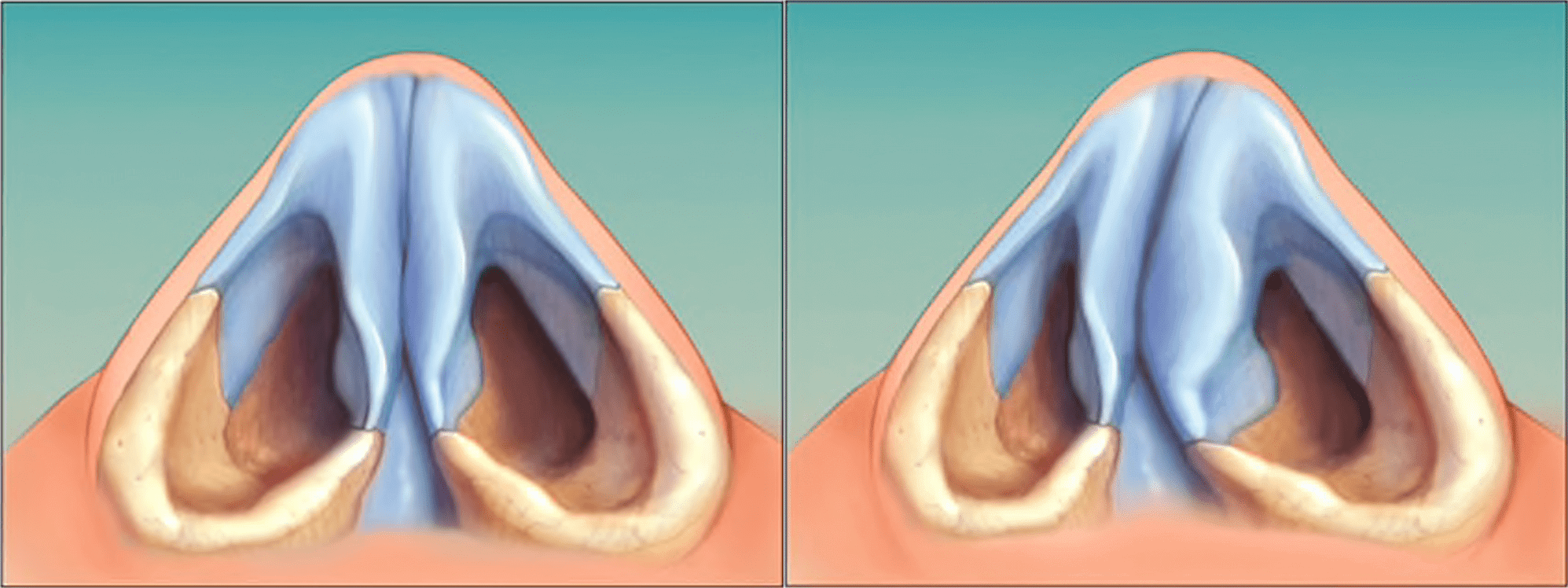
Figure 5. Deviation of the nasal septum.
Main factors contributing to the development of rhinosinusitis after sinus lift surgery:
- deviation of the nasal septum,
- neoplasms,
- foreign bodies,
- adenoids,
- polyps.
Many specialists consider it necessary to reduce the duration of rhinosinusitis treatment with timely therapy, namely: correction of nasal conchae, septoplasty. Obstructive changes in the nasal cavity and the paranasal sinuses significantly affect the prognosis, process, and quality of treatment; this is a pathogenetic factor of odontogenic maxillary sinusitis.
Pathology of the anatomical structures of the nasal cavity is the reason for the disruption of the self-cleaning mechanisms of the maxillary sinus, which predisposes to the development of inflammatory complications in the sinus after sinus lift surgery.
Thus, the pathological conditions of the paranasal sinuses and nasal cavity identified in the preoperative period of sinus lifting during the treatment of patients with mandibular alveolar ridge atrophy and dental arch defects complicate the course of subantral augmentation.
Defects of the maxillary sinus directly contribute to intraoperative difficulties during the surgical intervention - sinus lift surgery, which imposes additional requirements for conducting adequate preoperative examination, including endoscopic and radiological examination methods.
The above circumstances explain the necessity of researching and improving preoperative examination methods at the preoperative stage of sinus lifting, which is the basis for preventing most complications.
Complications of sinus lifting during and after the operation are presented in the webinar New Approaches to Sinus Lifting.
