Complications in Surgical Periodontology
Machine translation
Original article is written in articles.localeLanguage (link to read it) .
During any surgical intervention, including periodontal tissue, various complications can occur. To prevent them, it is necessary to strictly follow the indications and know the contraindications for each surgical technique.
A new approach to treating periodontitis is presented in the webinar Surgical periodontology without incisions. "Concept of Tissue Stretching".
Complications arise at different stages of surgical intervention, and they can all be grouped into the following categories:
- complications during anesthesia;
- tissue inflammation;
- retrograde pulpitis;
- bleeding;
- hematomas;
- wound edge separation;
- tooth mobility;
- swelling of surrounding tissues;
- tooth hyperesthesia;
- postoperative pain.
Let's discuss in more detail the complications mentioned above and consider ways to prevent them.
Complications during anesthesia
Today, thanks to the form of release of anesthetics, which are enclosed in cartridges (or ampoules), where the type of anesthetic, concentration of the solution, and other information are prescribed, the likelihood of injecting a substance other than the anesthetic or exceeding its dosage significantly is greatly reduced, but still exists.

Figure 1. Pain relief in dentistry.
Another serious complication at this stage is the patient's intolerance to the anesthetic, which in severe cases can lead to the development of anaphylactic shock. To prevent allergic reactions, it is important to thoroughly collect the patient's medical history, focusing on the patient's allergic status before starting the intervention. Any allergies to medications in the history should be noted in the outpatient card, specifying the name of the medication.
Complications are possible at the stage of direct administration of the analgesic drug if the doctor does not have clear knowledge of the anatomical-topographical characteristics of the injection area, made the wrong choice of anesthetic, the pain relief will be ineffective, or may not occur at all.
Inflammation of tissues
In the site of the surgical intervention, an inflammatory tissue reaction develops, the severity of which can vary. A common cause of this complication is neglecting the principles of antiseptics and aseptics or the absence of a gentle approach to the tissues of the surgical field. In the postoperative period, such patients are prescribed anti-inflammatory therapy, frequent copious rinses of the oral cavity with antiseptic solutions, antiseptic irrigation of the wound.

Figure 2. Surgical periodontology.
Retrograde Pulpitis
Occurs if there were teeth with healthy pulp in the area of surgical intervention, but during the operation, infection or trauma to the vascular-nerve plexus leading to the tooth occurred, causing symptoms of pulpitis. When retrograde pulpitis occurs, the causative tooth requires depulpation.
Bleeding
The source of bleeding in surgical periodontology can be the bone, its cancellous tissue, or soft tissues. Bleeding develops as a result of rough manipulations during the surgical intervention or against the background of the patient having problems with the blood coagulation system, the causes of which can be varied.
To achieve hemostasis, hemostatic clamps are used, sutures are applied to the mucous membrane, tamponade of the wound is performed by applying a hemostatic sponge or other hemostatic agents, and vessel ligation is carried out.
In case of damage to a major vessel, profuse bleeding, or inability to stop it over an extended period of time, parenteral administration of drugs to stop the bleeding is required.

Figure 3. Cause of bleeding.
For the prevention of this complication during surgical intervention, it is important to thoroughly collect the patient's medical history, establish the presence of blood coagulation system diseases, as coagulation disorders and blood diseases are contraindications for performing surgical interventions on the periodontium. If surgery is necessary for such a patient, a serious preparatory period is required with the mandatory involvement of a hematologist. This operation is performed in a hospital setting.
Hematoma
A hematoma is the result of damage to the integrity of a blood vessel of various diameters and the leakage of blood into the soft tissues. When a hematoma is detected, hypothermia is first applied, and then heat treatments are prescribed. In case of inflammation and suppuration of the hematoma, it is necessary to make an incision, and establish drainage.
Dehiscence of wound edges
Typically, this complication is associated with excessive tension of the wound edges or poor quality of suturing, or an insufficient number of sutures. To eliminate the consequences, the edges of the wound need to be refreshed, and the procedure of suturing should be performed again, only with adherence to all recommendations.
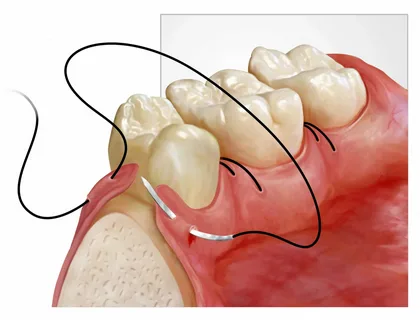
Figure 4. Applying sutures to the mucous membrane.
Tooth Mobility
In some cases, surgical intervention on the periodontal tissues, especially if it involved the bone substance of the alveolar process, is accompanied by the appearance of pathological mobility of previously immobile teeth. This complication requires the mandatory application of a splint. At the preparation stage for the operation, the development of pathological mobility can be predicted, in which case the splint is made in advance and then applied to the teeth, this can be done even before the start of surgical treatment.
Tissue Swelling
The appearance of swelling in the tissues around the jaw is caused by the body's reaction to surgical trauma and can be the result of rough execution of surgical intervention. To eliminate swelling, local anti-swelling therapy is necessary.
Tooth Hyperesthesia
During flap surgery or root surface curettage, mandatory treatment often leads to the formation of hyperesthesia of the hard tissues. This can also be associated with postoperative exposure of the roots. This complication requires the implementation of remineralizing therapy and covering the teeth with fluoride-containing agents. Electrophoresis with remineralizing agents is highly effective. Patients are selected toothpastes to correct tooth sensitivity.
Sometimes, curettage is accompanied by profuse bleeding, significantly complicating the visibility of the surgical field. As a result, fragments of hard dental deposits, stones, may not be washed out from the intervention area during antiseptic irrigation, and can embed deeper into the soft tissues. Consequently, this may lead to the infection of the periodontium, and in severe cases – abscess formation.

Figure 5. Inflammation in the intervention area.
Another mistake that can lead to serious consequences is performing surgery against the background of a pronounced inflammatory response. First, conservative treatment should be carried out. Sometimes, to suppress the inflammation, it is sufficient to open a periodontal abscess, and in some cases, it is necessary to remove the causative tooth.
Postoperative Pain
This is the most common complication of any surgical intervention, which is managed by taking analgesics. To prevent complications and optimize reparative processes in the postoperative period, the patient must carefully follow individual hygiene. During the first week after the surgery, the patient uses a soft brush and therapeutic-prophylactic pastes. For activating the healing processes, laser therapy is effectively used.
Conclusion
The effectiveness of any surgical intervention is determined by the presence of indications for its implementation, taking into account the form of the disease, the depth of the lesion, the characteristics of the gingival margin, the degree of resorption of the alveolar bone, the presence of pathological processes in the area of root furcation, the level of root surface exposure, and the general health condition of the patient.
Patients after surgery are subject to mandatory dispensary observation, which involves monitoring the general and local status. The dynamics of the process are assessed by the following indicators: condition of the gingival margin, periodontal indices, presence of periodontal pockets and their depth, capillary resistance, tooth mobility, radiological picture, osteometry, and immune status. The main criteria for the condition of the periodontal tissues are: positive dynamics, stabilization, negative dynamics, no changes. The frequency of examinations depends on the stage and severity of the process, the presence of underlying pathology, and the reactivity of the organism.
Protocols for non-surgical periodontal treatment in the online course Masterclass on Surgical Periodontology: Techniques and Innovations.

/public-service/media/default/117/fY2Ps_653115953b491.jpg)
/public-service/media/default/119/VHujO_653115c371283.jpg)
/public-service/media/default/112/Kg3LQ_65311525c7da9.jpg)
/public-service/media/default/438/vwHtT_671a16efda90f.png)