Anatomical Rationale for Sinus Lifting
Machine translation
Original article is written in RU language (link to read it) .
Dental implantation in dental practice is a reliable method of rehabilitation for patients with complete or partial adentia. The main factor preventing implantation in the upper jaw is the lack of bone volume on the lateral parts of the alveolar ridge. In some cases, this is due to the anatomical and topographical characteristics of the patient's maxillary sinus, among which the following can be highlighted:
- periodontal diseases,
- systemic or local osteoporosis,
- atrophy of the alveolar ridge after tooth extirpation,
- high pneumatization of the sinus.
Preparing the patient for sinus lifting at the webinar Open and Closed Sinus Lifting: Detailed Protocols.
Topographic and Anatomical Characteristics of the Maxillary Sinus
For successful dental implantation, a doctor must possess complete knowledge of the anatomy of the jaw, the structure and topography of bone formations, and their age-related characteristics.
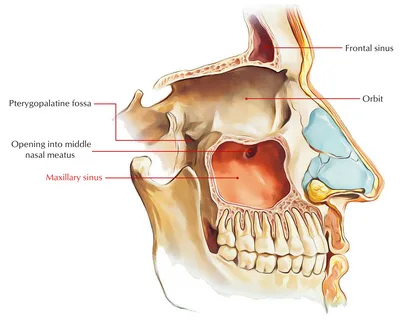
Figure 1. Maxillary sinus.
The maxillary sinus is the largest of the paranasal sinuses by volume; its configuration resembles a pyramid, and its volume reaches 20 mm³. During sinus lifting, the following parts of the sinus are of greatest importance to the doctor:
- the floor,
- the medial wall,
- the anterior wall.
In half of the patients, there is a bony depression at the floor of the maxillary sinus called the alveolar recess, and in a quarter of the patients, there may be a complete or incomplete septum located here. The presence of such a bony septum significantly complicates the detachment of the mucosal flap and the elevation of the Schneiderian membrane, which may be accompanied by its perforation.
Types of Maxillary Sinus Structures
There are several types of maxillary sinus based on their characteristics.
- The pneumatic type is characterized by a large sinus volume, often extending below the apices of the roots and the floor of the piriform sinus, including bays or protrusions in various directions. This type often contains additional bony septa.
- The sclerotic type is characterized by a relatively small sinus volume, with the sinus floor located away from the root apices, above the nose, and lacks protrusions.
- The mixed type of sinuses is characterized by a medium volume, with the sinus floor located in the area of the root apices, slightly below or at the level of the nasal floor. Protrusions are rare.
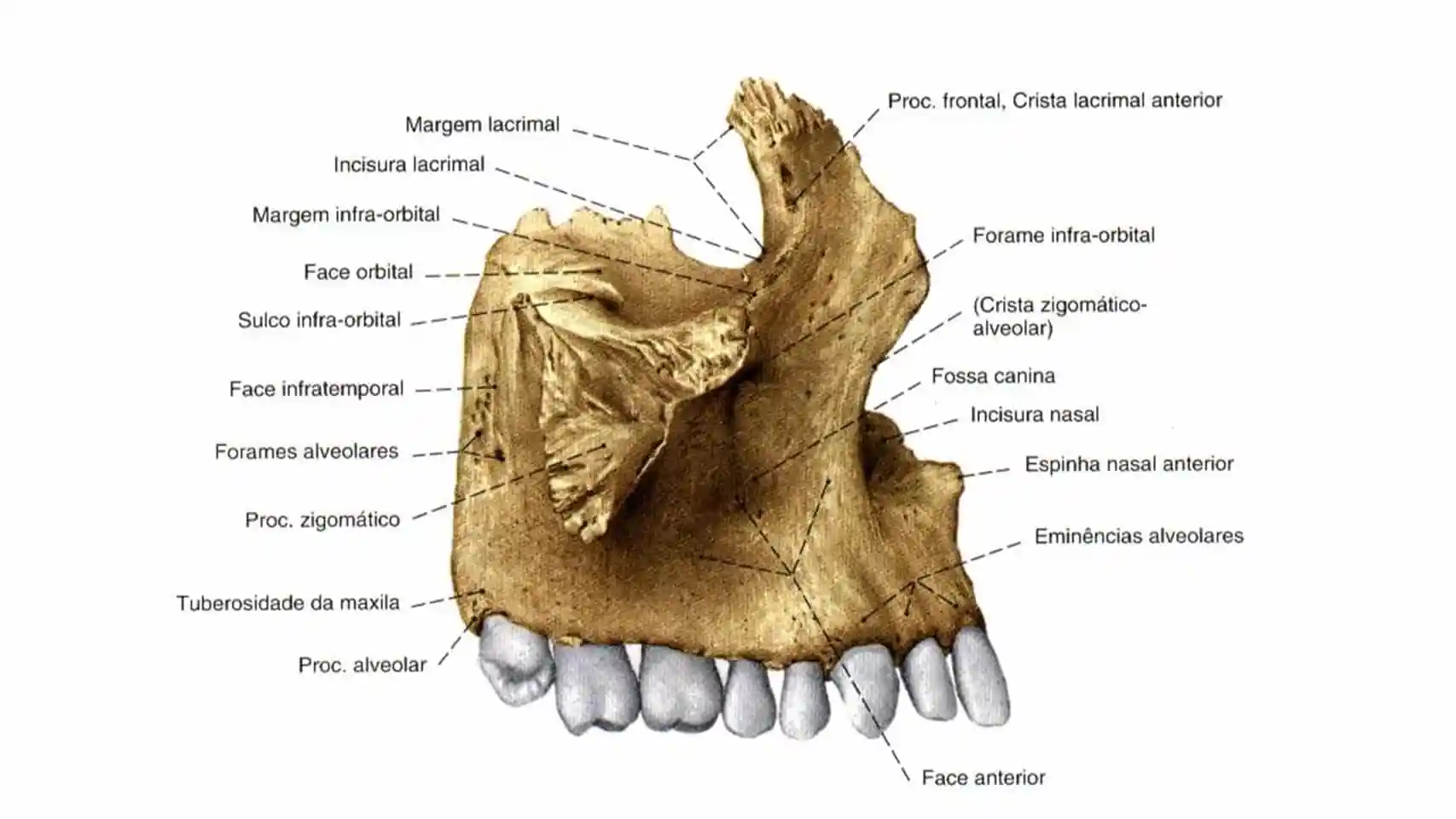
Figure 2. Structure of the upper jaw.
Age-related changes
Practicing physicians need to consider the age-related anatomical changes occurring in the maxillary sinus.
After the age of 30-40, initial signs of changes appear, processes of osteoporosis in the cancellous bone predominantly in the area of the sinus floor begin, and atrophy of the alveolar ridge along its lower edge starts.
After the age of 50-60, the thinning of the walls becomes more noticeable, largely influenced by the number and timing of tooth extractions on the upper jaw.
Anatomical structure
The anterolateral wall is represented by a thin cortical layer, where a vascular-nerve plexus runs, an arterial anastomosis is located, which in half of the patients is situated on the surface of the bone, a few centimeters from the edge of the alveolar process. In the other half of the patients, the vessels are located inside the bone tissue. It is important to avoid damaging this anastomosis during the open method of sinus lifting, during the formation of the bone "window", as this will lead to a serious complication – severe bleeding.
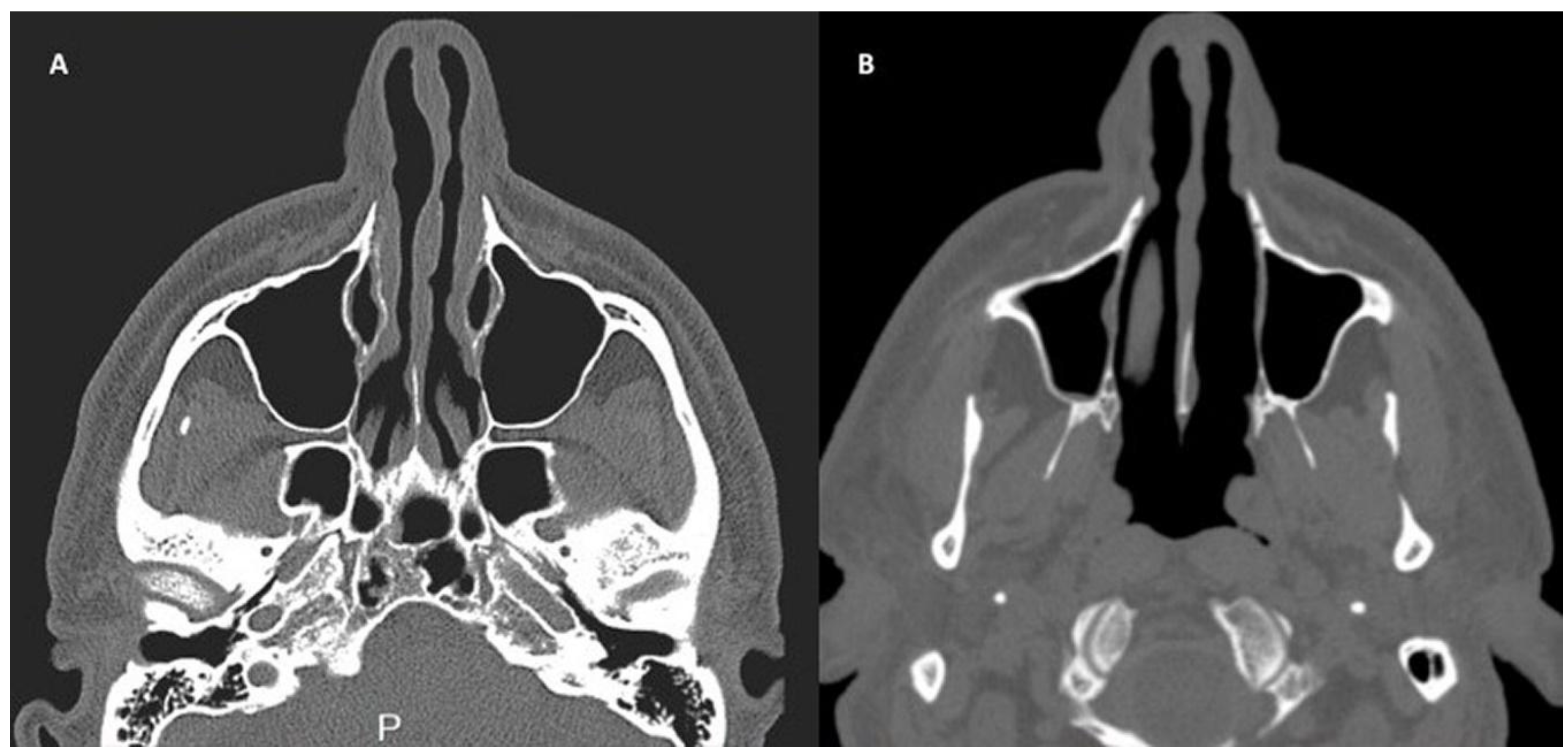
Figure 3. Computed Tomography.
The medial wall of the sinus is represented by the frontal process of the jaw. In the upper-outer part of the sinus, 2-3 above the floor, there is a natural ostium through which drainage and aeration of the sinus are carried out. Normally, the size of the ostium is 5 by 10 mm, it opens into a semilunar slit, which is bordered anteriorly by the uncinate process, medially by the anterior part of the middle nasal concha, and posteriorly by the ethmoid bulla. These bony formations form the osteomeatal complex, located in the initial section of the middle nasal passage – this is a crucial section that determines the general condition of the paranasal sinuses, their anterior group.
The osteomeatal complex was first described by H. Naumann in 1965. Understanding the localization of the drainage opening during surgical intervention helps the surgeon to perform more precise manipulations in this area to prevent damage to the drainage and ventilation functions of the sinus.
The next important anatomical structure is the middle nasal concha, which is a medial projection of the lateral wall of the nasal cavity, hanging over the hook-like process, ethmoidal bulla, and semilunar hiatus. Anteriorly and superiorly, this structure is connected to the perforated plate, whereas in the anteroposterior direction, its free edge hangs in such a way that the caudal end is below the sphenopalatine fossa. Normally, the hook-like process begins in the area where the middle nasal concha attaches, continues obliquely downwards and backwards, reaching the upper part of the lower nasal concha. The ethmoidal bulla is located a few millimeters backwards.
The nasal mucosa was first described in detail in the 17th century by the German anatomist Shneider C.V., who also established its structural similarity to the mucosa lining the maxillary sinus. Later, Shneider C.V. compiled a detailed description of the mucosa of the maxillary sinus, which was subsequently named the "Shneiderian membrane".
Schneider's membrane is a mucous membrane that lines the floor of the maxillary sinus, its thickness is small, about 0.1-0.5 mm, consisting of several layers, topped with pseudostratified columnar epithelium, which includes the following types of cells: goblet, intercalated, and ciliated epitheliocytes. On the surface of any of the ciliated cells, there are up to 200 cilia, which are surrounded by the thinnest layer of periciliary fluid, and above them accumulates mucus, produced by glands located in the own layer of the mucosa and by goblet cells.
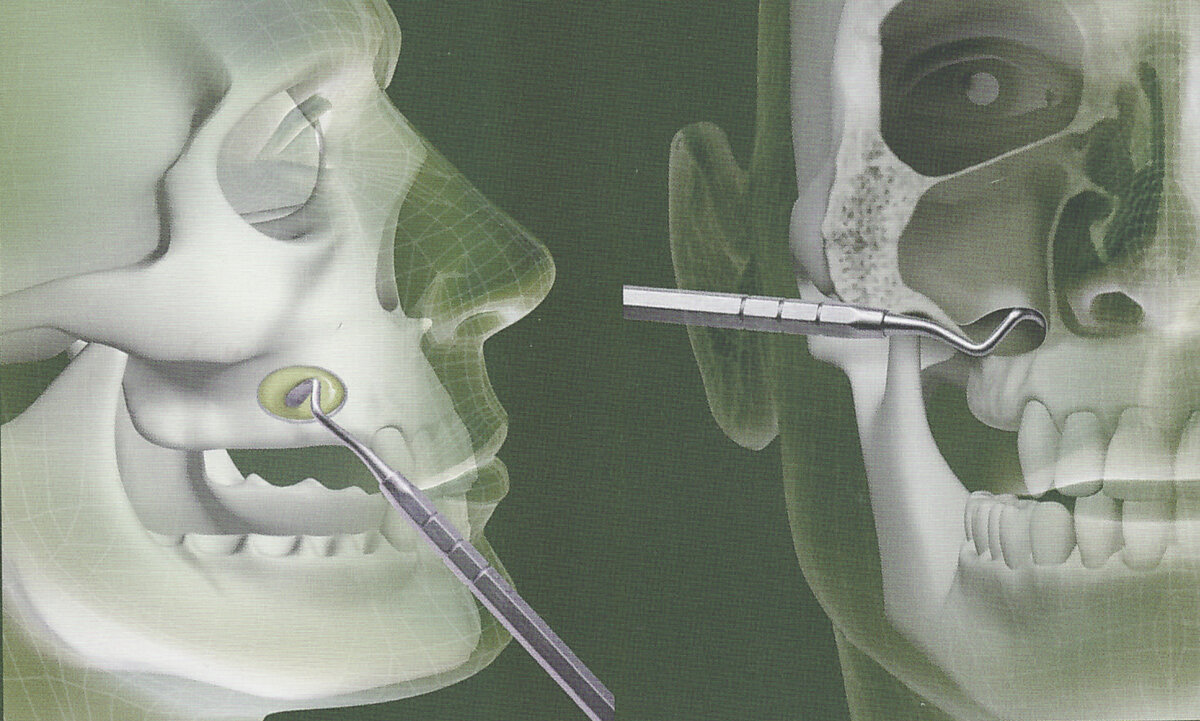
Figure 4. Access during sinus lifting.
Connective tissue is the main component of the mucosa's own layer, it includes many fibers of different types: collagen, reticular, elastic. Vessels and nerves run between the fibers, mucous glands and cellular elements are located here: histiocytes, eosinophils, plasma cells, mast cells, and lymphoid cells.
The secretion produced by goblet cells, as well as by endothelial glands located in the mucosa of the paranasal sinuses and nose, consists of 96% water, and also includes glycoproteins, prostaglandins, immunoglobulins, and lactoferrin. The ciliated epithelium performs the function of breathing, which is carried out in the sinus thanks to the diffusion of oxygen from the inhaled air, since the volume of air coming from the blood is insufficient, which confirms the importance of aeration.
Air enters the paranasal sinuses on exhalation, this is due to the direction of the anatomical openings of the sinuses inward and backward to the choanae, and the suction of fresh air leads to its movement in the olfactory area. The pressure in the paranasal sinuses is lower than in the lungs or nasal cavity. Due to the narrow nasal passages, the pressure equalizes very slowly. In the nasal cavity, on inhalation, the pressure decreases and the moistened, warmed, purified air partially exits from the paranasal sinuses into the nasal cavity, mixing with the main stream. The vortices that occur at this stage in the upper part of the main jet come into direct contact with the olfactory zone, responsible for the perception of smells.
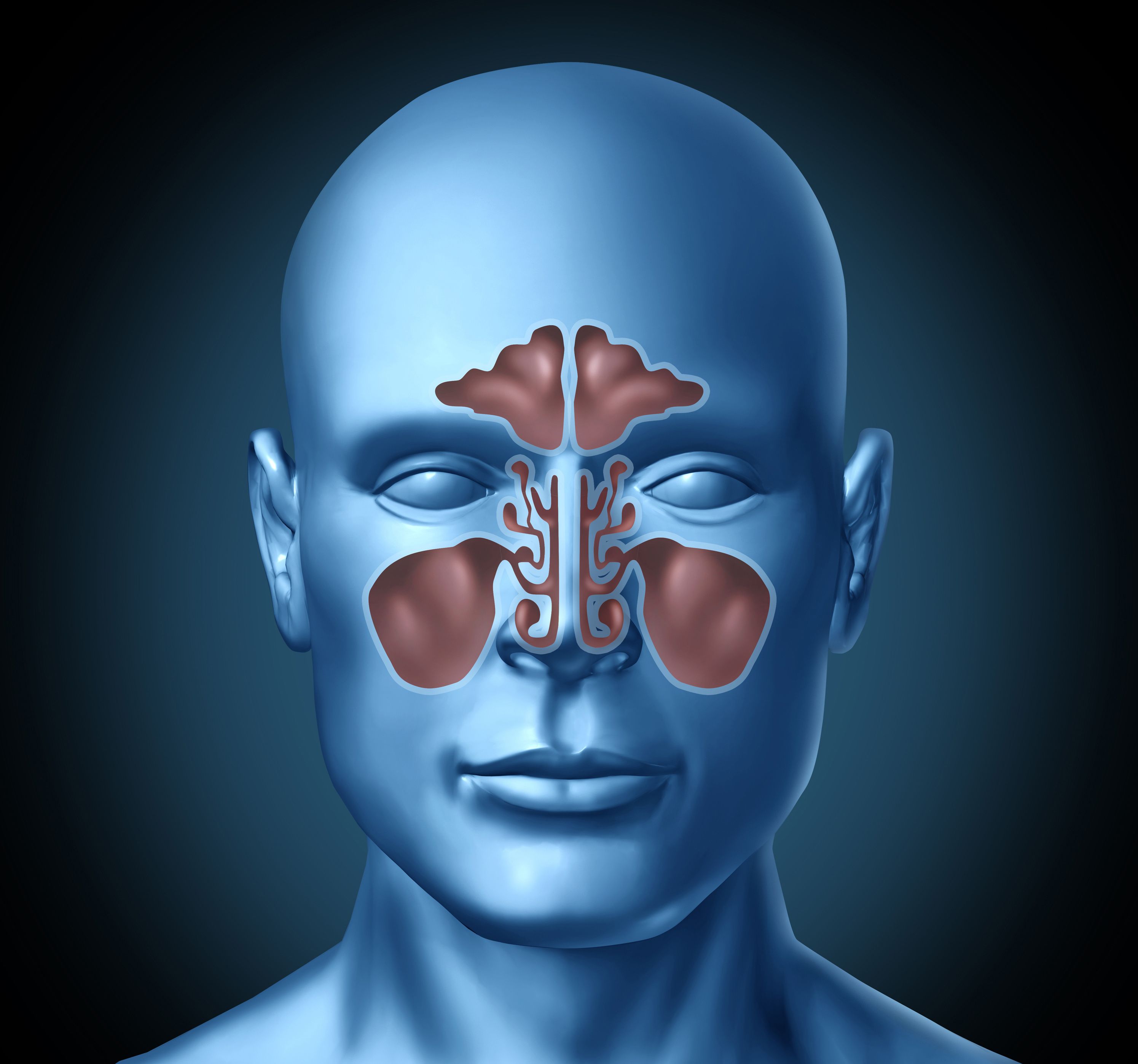
Figure 5. Connection of sinuses.
As a result of the inflammatory process, which is accompanied by pronounced swelling of the mucosa of the upper jaw, the diameter of the anatomical opening decreases, which causes difficulty in performing the drainage and ventilation functions of the paranasal sinuses. The single-layered multi-row epithelium, which normally lines the mucosa of the sinus, is gradually replaced by connective tissue due to chronic inflammation.
The knowledge of histological, anatomical, and physiological characteristics of the maxillary sinus requires the surgeon to be careful and cautious during surgical intervention in this area, in order to avoid perforation of the mucosa of the maxillary sinus during its detachment in the course of the operation.
The anatomy of the maxillary sinus is presented in the webinar Sinus lifting techniques: lateral and transcrestal approach, Intralift technique.
