Principles of Radiation Therapy
Machine translation
Original article is written in RU language (link to read it) .
Radiation therapy is primarily used for local impact directly on the tumor focus, as well as on the area of regional metastasis. Before undergoing radiation therapy, all patients with head and neck neoplasms must undergo oral cavity sanitation.
Always up-to-date information on the treatment of maxillofacial diseases can be found in the section Education on Oral and Maxillofacial Surgery.
If a patient needs to have teeth removed near the radiation area, in such a case, the wound from the surgical intervention must fully heal before the start of radiation.
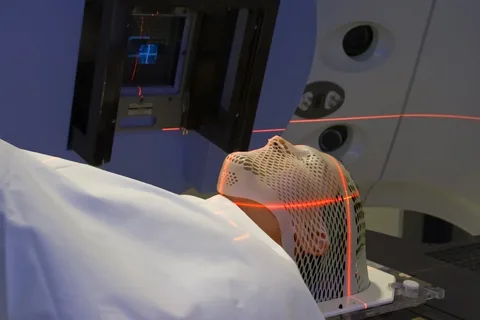
Figure 1. Radiation therapy for head neoplasm.
Radiation therapy for malignant neoplasms is based on the biological effects of ionizing radiation. The degree of morphological transformations in cells under radiation exposure is determined by the following factors:
- degree of cell differentiation,
- activity of metabolic processes,
- mitotic activity of cells.
In this case, there is such a dependency: the less differentiated cells, which have high mitotic activity and active metabolic processes, are most radiosensitive.
The tumor tissue is heterogeneous in oxygen, consisting of chaotically arranged areas of cells with varying degrees of oxygenation — increased at the periphery, but anoxic in areas that lack normal blood supply (central part of the tumor, where decay is concentrated).
Radiosensitivity
The radiosensitivity of tissues directly depends on the oxygen pressure within them. Compared to highly oxygenated cells, hypoxic cells are more radioresistant and continue to be a source of ongoing tumor growth despite treatment.
Tumors, depending on their response to radiation exposure, can be classified as follows:
- radiosensitive, which include lympho- and reticulosarcoma, lymphogranulomatosis, basal cell carcinoma;
- moderately radiosensitive, this group includes various forms of squamous cell carcinoma;
- radioresistant tumors (fibro-, chondro-, neurosarcomas, osteogenic sarcomas);
- moderately radioresistant (adenocarcinoma).
The goal of radiation therapy is not only to achieve a cure but also to maximize the preservation of function and morphology of the irradiated organ. In the case of radiosensitive forms, the destruction of the neoplasm is carried out without harm to the healthy surrounding tissues. For radioresistant forms, higher doses of radiation are required, which negatively affect healthy tissues. Therefore, radiosensitivity is synonymous with the susceptibility of the irradiated area.

Figure 2. Radiation therapy device.
The tumor's response to radiation is determined by the following factors:
- growth pattern (exophytic tumors have greater radiosensitivity compared to infiltrating or ulcerative ones);
- histological structure, level of cell differentiation;
- growth rate (fast-growing tumors are more susceptible to radiation than tumors with a slow growth rate);
- blood supply, with good blood supply the tumor is more radiosensitive;
- structure of the tumor, formations with edematous stroma, rich in collagen fibers are more radioresistant than tumors whose stroma contains many lymphocytes and eosinophils;
- the center of the tumor is more radioresistant than the periphery;
- the addition of inflammation increases the radiosensitivity of healthy tissues but decreases the sensitivity of the tumor.
Radiation therapy as a treatment method
There are various protocols for using radiation therapy in the treatment of malignant head and neck tumors:
- as an independent method of treatment;
- combination with surgical intervention;
- in conjunction with chemotherapy and hormone therapy;
- multimodal therapy.

Figure 3. Preparing the patient for radiation therapy.
If we talk about radiation therapy as an independent treatment, it can be carried out according to a radical program, used as palliative or symptomatic techniques.
- Radical therapy involves the total suppression of the viability of the neoplasm by creating in the primary focus the necessary dose of radiation for the destruction of the tumor.
- Palliative therapy is conducted to slow the growth of the tumor, reduce its size, minimize accompanying symptoms, and improve the quality or prolong life.
- Symptomatic radiation therapy is used to eliminate or reduce the intensity of clinical symptoms that can cause imminent death of the patient or significantly worsen the quality of life.
A combined approach, using radiation therapy in conjunction with surgical intervention, can be applied at the following stages:
- preoperative;
- intraoperative;
- postoperative.
Indications for preoperative radiation:
- devitalization of all radiosensitive cells within the tumor;
- reduction in the size of the neoplasm due to regression of the most radiosensitive elements at the periphery;
- suppression of mitotic activity of tumor cells;
- obliteration of small lymphatic and blood vessels;
- prevention of metastasis and recurrence.
Indications for postoperative radiation:
- in cases of non-radical surgical resection of the tumor focus;
- if ablative procedures are not followed;
- when tumor cells are found in the marginal sections of the excised tissues;
- to eliminate malignant tissues in regional lymph nodes.
Intraoperative use of ionizing radiation is indicated for a single use immediately before tumor excision (preoperative option) or (postoperative option) irradiation of the malignant element that remains after non-radical removal, or in the case of an unresectable tumor.
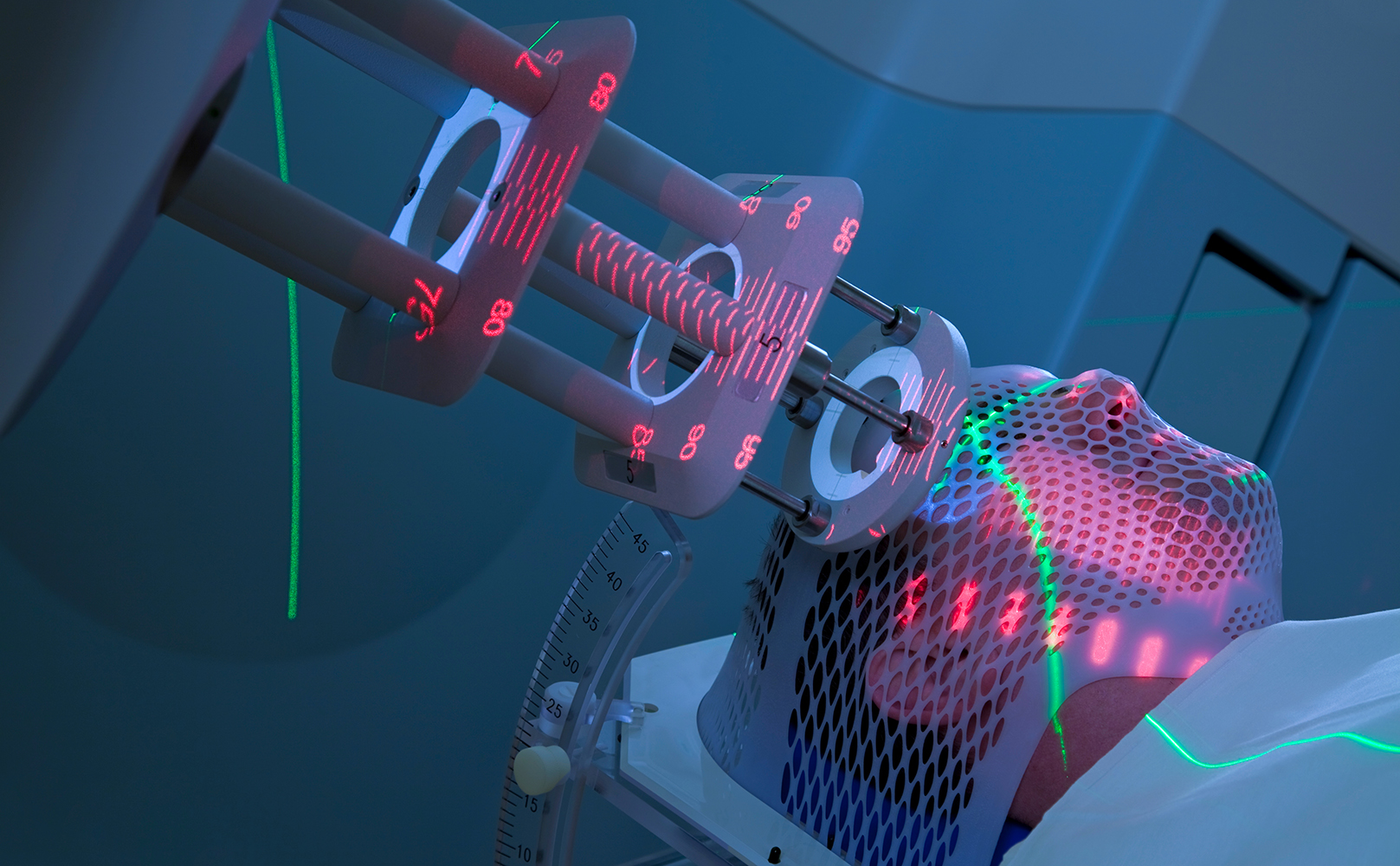
Figure 4. Use of gamma radiation.
A combined method of treatment involves the use of radiation and pharmacological therapy in inoperable patients, in the presence of reticuloendothelial lesions.
Multimodal therapy includes the use of modern techniques of surgical, radiation, and pharmacological treatment, combining them with other methods that have a radiomodifying effect (hyperbaric oxygenation, hyperthermia).
Contraindications for radiation therapy
There are some contraindications for the use of ionizing radiation:
- risk of worsening the patient's condition as a result of radiation therapy against the background of multiorgan pathology;
- if a previously conducted radiation course was ineffective, a recurrence occurred, a repeated course of radiation therapy will not be effective.
Radiation methods
Today, existing radiation techniques by the method of delivering ionizing radiation to the pathological focus can be divided into:
- external, in turn, are subdivided into (contact and distance);
- internal (systemic and brachytherapy).
Remote radiation exposure can be performed statically, or through moving irradiation.
Static irradiation is performed thanks to shaping devices (wedge filters, protective blocks). They are necessary to create the maximum difference in doses absorbed by the surrounding healthy tissues and the primary tumor focus.
In the case of moving irradiation, the irradiated object and the source of ionizing radiation are in motion.
Contact methods
The representative of contact radiation therapy is the applicator method, which has proven itself well in clinical situations where the malignant neoplasm is located at a shallow depth and does not infiltrate adjacent tissues. The radioactive substance in applicator beta-therapy is placed at a distance of 5 mm from the skin or mucous membrane.
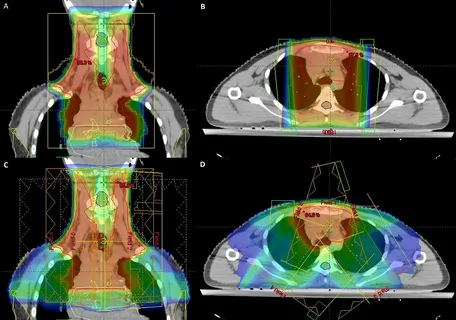
Figure 5. Planning radiation therapy in the neck area.
Contact gamma therapy is indicated if the tumor process infiltrates the underlying tissues or skin. In this case, the depth of infiltration must be more than a few centimeters. The distancing is 0.5-5 cm. This technique is used independently for skin cancer, lip cancer, and also for mucosal cancer in combination with external gamma therapy.
Internal Radiation
It involves the introduction of a radioactive radiation source directly, it can be divided into treatment with closed radioactive sources (brachytherapy) and open (systemic therapy).
Intratissue gamma therapy is indicated for cancer of the lip, skin, tongue, mucous membrane. Intracavitary irradiation (the radiation source is located inside the patient's natural cavity), intratissue irradiation (the location of the radiation source is in the body tissues).
When planning radiation exposure, it is important to accurately assess the area of irradiated tissues. The volume of irradiation fields depends on the extent of the pathological focus and the morphological structure of the tumor.
Find a lot of useful information on various sections of dentistry on the website ohi-s.com.
