Clicking jaw
Machine translation
Original article is written in RU language (link to read it) .
Jaw clicking is a condition that in most cases is caused by a disruption in the coordination of movements of the lower jaw head and the articular disc (internal pathology of TMJ), characterized by the appearance of various types of noise (crackling, clicking, popping) when opening or closing the mouth, and changes in the jaw's range of motion at different stages of its movement.
About the norm and pathology of the temporomandibular joint in the webinar TMJ Dysfunction: A Modern View on the Problem (Part 1).
This pathology occurs among both adult and child patients. According to ICD-10, this disease is coded as K07.61.
Today, several nosological forms of internal TMJ lesions are recognized, which can cause the appearance of noise phenomena such as clicking in the area of the joint head during jaw movement. These include the following clinical forms of TMJ pathology:
- subluxation of the articular disc;
- recurrent dislocation of the articular disc;
- chronic dislocation of the lower jaw head with subluxation of the articular disc;
- chronic dislocation of the articular disc;
- chronic posterior dislocation of the articular disc.
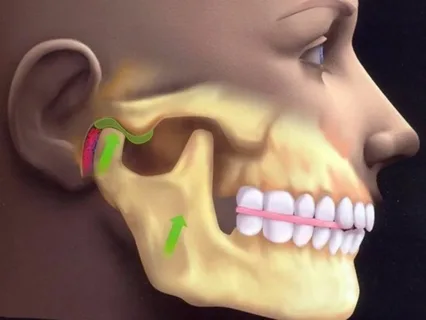
Figure 1. Joint pain.
Etiology
Several causative factors that provoke jaw clicking can be identified, including:
- Increased tone of the masticatory muscles. Clicking occurs during the contraction of muscle fibers while performing chewing movements, particularly when it is necessary to chew relatively hard food. In more rare clinical cases, a pathological spasm caused by previous excessive load, stress, or inflammatory processes is observed.
- Traumatic injury. As a result of external force application (a powerful directed blow to the joint area from the right or left), the anatomical structure of the joint changes: the integrity of the cartilage is disrupted, the meniscus is crushed, and the joint head is dislocated or subluxated.
- Caries lesions, predominantly localized on one side of the dental arch, eventually lead to different bite heights on opposite sides of the jaw, causing pathological mutual positioning of the joint elements.
- Bruxism – a condition where the patient involuntarily moves their jaw, accompanied by teeth grinding, predominantly during sleep. According to literature, this problem occurs in approximately 10% of the population. The pathology is caused by spasms of the masticatory muscle fibers.
- Consequences of poor-quality dental care. This includes orthopedic treatment, improperly installed artificial crowns, and implants that cause bite disturbances, and as a result, lead to TMJ dysfunction.
- Joint fatigue due to being in the same position for an extended period of time. Example: keeping the mouth open for a long time during dental treatment. To prevent this condition, it is recommended to allow patients to rest a bit when the treatment protocol permits.
- Arthritis – an inflammatory joint disease, predominantly caused by bacterial microflora.
- Osteoarthritis – a pathology that develops due to the thinning and gradual destruction of the cartilage surface and joint disc, along with these changes, compensatory growths are also observed.

Figure 2. The patient complains of pain when opening the mouth.
Clinical Manifestations
The following clinical symptoms are characteristic of the condition known as clicking jaw:
- Sound manifestations of varying intensity are typical even at the initial pathological changes in the joint, these can be joint clicks or noise.
- Sound manifestations sometimes appear as crunching or crepitation, clicks.
- Sound phenomena are diagnosed either at the very end of the mouth opening act, or at the very beginning of the mouth closing process, when the head of the lower jaw moves to the anterior slope of the articular tubercle.
- The patient may complain about the presence of joint noises over a fairly long period of time (often for several years), but does not seek help due to the absence of pain.
- Often, the reason for seeking help becomes the fact that joint sound phenomena begin to attract the attention of others, which brings significant discomfort and complicates the patient's life.
- The appearance of sound phenomena can be diagnosed in patients suffering from malocclusions, as well as individuals with orthognathic bite, who do not have occlusional disturbances.
Disease Diagnosis
During the clinical examination, the following symptoms are detected:
- Clicking sounds are heard when the joint head moves within the joint socket.
- Acoustic phenomena are determined at both stages of movement: opening and closing the oral cavity.
- If the patient is asked to open their mouth to the maximum, the joint head does not leave the joint cavity. This pathological condition is called a subluxation of the joint disc.
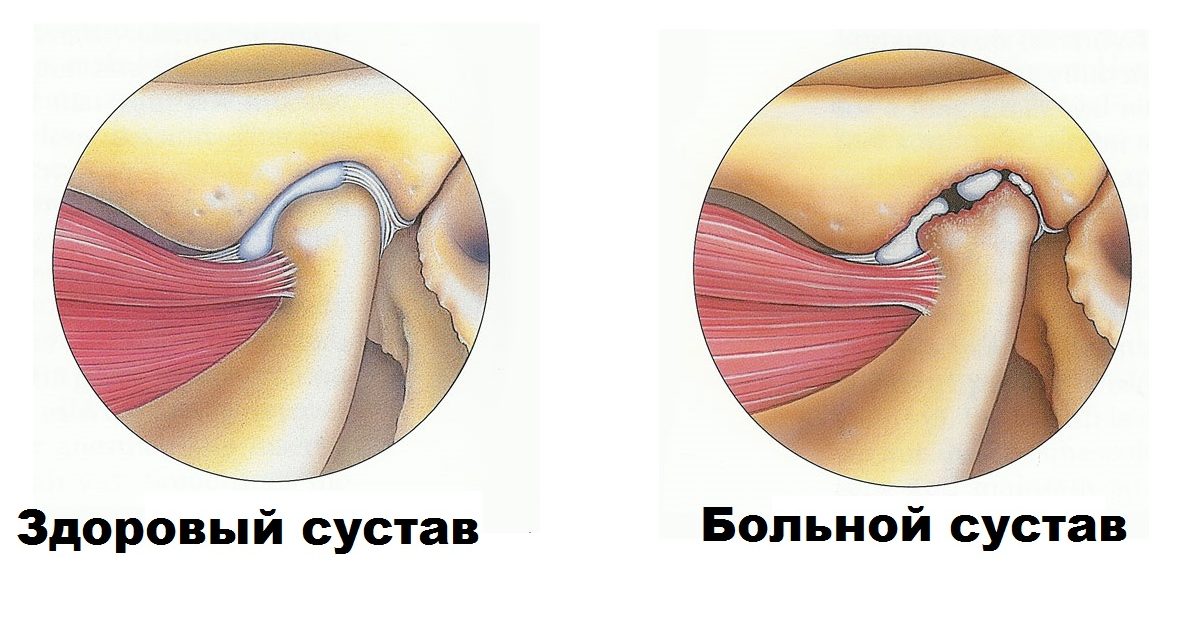
Figure 3. Diagnosis of joint pathology.
If the clinical symptoms worsen as the disease progresses, there is an intermittent, irreducible displacement of the joint disc, which clinically is accompanied by periodic locking of the temporomandibular joint. The duration of the locking can last several minutes, or it may reach many hours. Subsequently, the disc is repositioned, sometimes this process is spontaneous, but in some cases, the patient's assistance is necessary; by moving the lower jaw in various directions, he achieves repositioning. This condition is called recurrent dislocation of the joint disc.
As the pathological process develops further, the ability of the ligamentous apparatus of the bilaminar zone to regulate the spatial position of the joint disc is completely lost, the predominance of contractions of the external pterygoid muscle, which provides the forward and inward displacement of the disc, becomes habitual, leading to permanent joint locking. Clinically, this manifests as a limitation of mouth opening to a maximum of a few centimeters between the cutting edges of the incisors, accompanied by pain sensations and a feeling of obstruction in the joint when attempting to open the mouth, and displacement of the jaw to the uninjured side. Lateral movements of the jaw to the opposite side are limited, and these movements are often sharply painful.
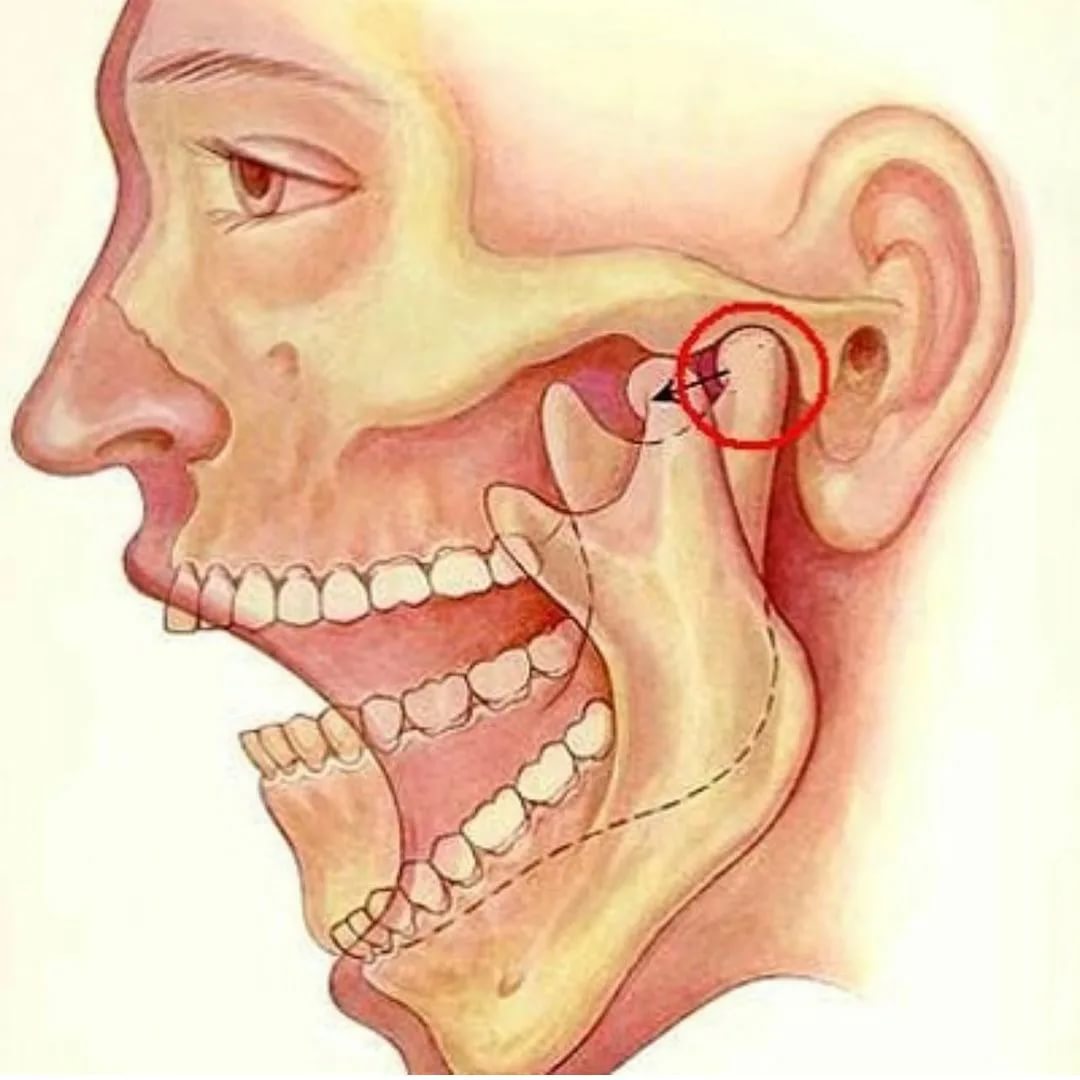
Figure 4. Phases of mouth opening.
If the anterior displacement of the meniscus is not corrected within six months from the onset of the first symptoms, symptoms of adhesion join the deformation, occurring as a result of the progression of the adhesive process, and the clinical picture resembles secondary osteoarthritis. In addition to the locking of the lower jaw, there are painful sensations in the area of the damaged joint not only during any function but even at rest.
Rear dislocation of the joint disc, unlike the anterior, is extremely rare. It is characterized by the following clinical manifestations:
- there is no dense multiple contact between the teeth, the teeth may not come together on the affected side,
- even an attempt to tightly clench the teeth causes sharp pain in the patient,
- clinical examination reveals entrapment of the disc between the posterior surface of the joint fossa and the joint head.
The causes of clicks in the joint are the pathology of coordinated movements of the joint disc and the joint head on one side, or bilateral disturbance, displacement, and various deformations of the disc. Changes in the mutual position of the joint elements, the lack of coordination in the movements of the disc and the head cause entrapment of the disc, complicating the mobility of the lower jaw.
Differential Diagnosis
It is necessary to distinguish a clicking jaw from chronic dislocation.
Palpation in chronic dislocation shows smooth sliding when opening the mouth of the jaw head with exiting from the joint fossae.
Radiologically: the disc is normally positioned relative to the jaw head in any phase of movement.
In the history of habitual dislocation, there is always an acute dislocation, and its reduction was performed by the patient themselves or a medical worker.
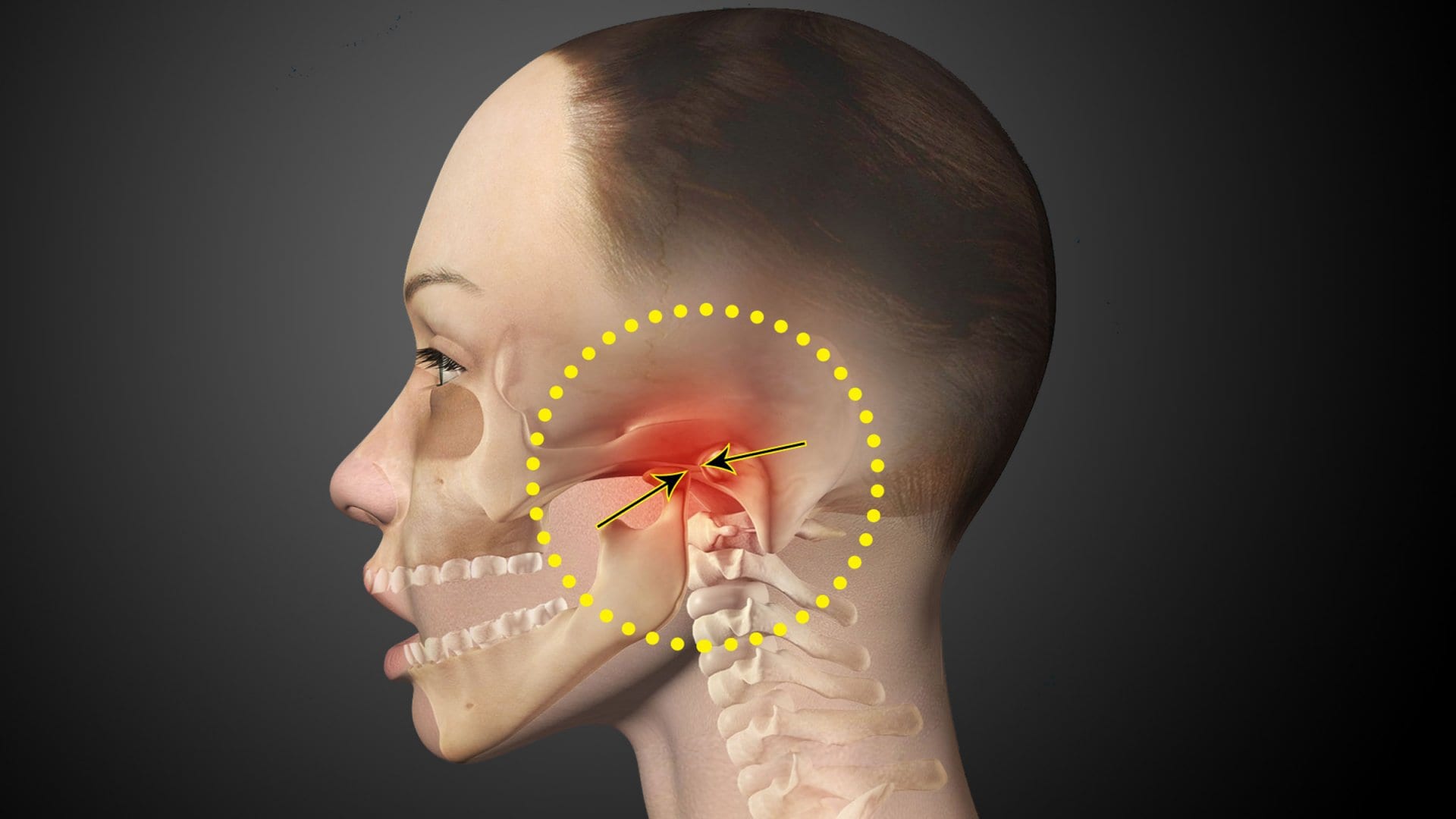
Figure 5. Locking of the lower jaw.
Therapy Principles
The goal of treatment is to eliminate noise (sound) phenomena in the joint area by normalizing the intra-articular mutual positioning of the anatomical structures of the temporomandibular joint to prevent recurrence of the disease. The target group includes both adult patients and children.
Effective treatment and achieving a positive result is only possible in the case of comprehensive treatment, involving a number of specialists: a surgeon, physiotherapist, orthodontist, orthopedic dentist, psychiatrist, and a physical therapy specialist.
The diagnostic criteria for musculoskeletal dysfunction are presented in the webinar Principles of Diagnostics of Musculoskeletal Dysfunctions.
