Complications of dental implantation
Machine translation
Original article is written in RU language (link to read it) .
Dental implantation ensures the restoration of the continuity of the dental row, proper physiological load distribution on the remaining teeth, normalization of impaired speech and chewing functions, improvement of the patient's psychological state and aesthetics, and opens new horizons for increasing the quality of dental care.
More relevant information on this topic at the webinar Complications in implantation and techniques for their elimination.
A predictable treatment outcome can only be achieved with careful planning, taking into account all the features and mechanisms of bone regeneration, provided that a team of specialists works together: a periodontist, surgeon, orthopedist, and dental technician.

Figure 1. Radiological signs of peri-implantitis.
Today, a huge variety of implants are produced, differing in configuration and application technique, which is consistent with the multimodal concept of dental implantation.
In their main function of supporting orthopedic structures, endosseous implants can last for about 30 years, and there are known cases of even longer duration.
However, the use of an implant over a long period is not the only criterion for the effectiveness of the treatment performed.
The indicators of effective dental implantation can be highlighted as follows:
- maintenance of clinical stability under the influence of functional
load (no mobility and inflammatory phenomena in the adjacent tissues); - absence of pain and any unpleasant sensations in patients;
- no signs of bone resorption in the area of the implant;
- bone tissue of the alveolar ridge atrophies in the area of the dental implant at a rate not exceeding 0.2 mm per year.
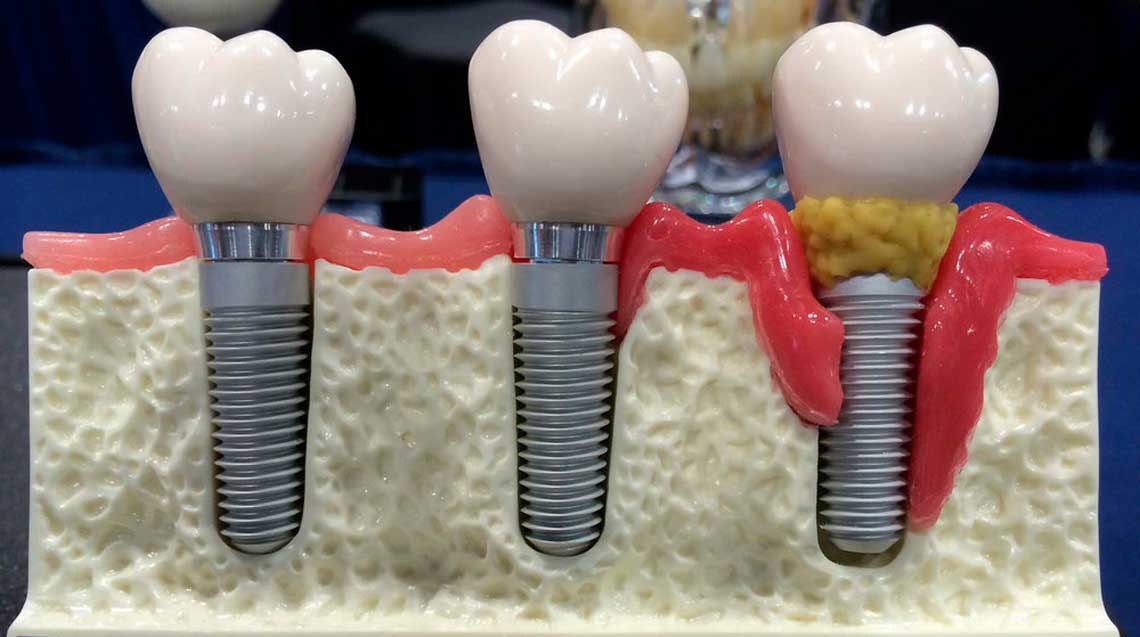
Figure 2. Implant rejection.
The indicators presented above allow us to assess the level of preparedness of specialists, as well as to determine the quality of the dental implants themselves.
Complications of the Surgical Stage of Dental Implantation
Among the most common biological factors contributing to complications after the surgical stage, the following should be highlighted:
- insufficient blood supply to the bone tissue fragment in the implant area,
- local osteoporosis,
- general diseases of the patient, which were not timely identified, causing disturbances in osteogenesis.
However, it should be noted that in the vast majority of clinical situations, complications are related to errors at the stage of patient selection, in the process of planning the upcoming treatment, performing the surgical intervention, or directly during prosthetics.
The most common complications associated with the course of dental implant surgery:
- fracture of the guide drill or bur;
- damage to nerve fibers;
- bone burn during dissection;
- perforation of the floor of the maxillary sinus, damage to the mucous membrane;
- bone fracture;
- primary fixation was not achieved.
The above complications are the result of excessive mechanical impact, incorrect determination of the height of the alveolar ridge by orthopantomogram, and improper technique of forming the bed.
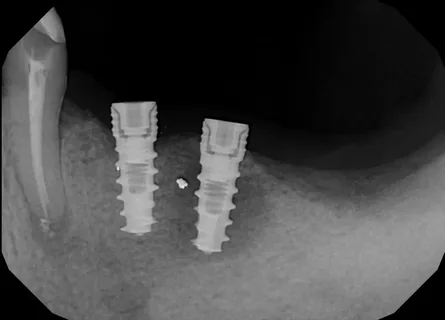
Figure 3. Signs of peri-implantitis.
Gradual accumulation of practical clinical experience will help reduce the complication rate of dental implant surgery to 1-2% of cases.
Complications of the postoperative period of dental implantation
As a rule, these complications are diagnosed within the next 10 days. The following complications can be identified for the postoperative period:
- bleeding,
- hematomas,
- pain sensations,
- suture dehiscence,
- inflammatory phenomena in the surrounding soft tissues of the jaw (periostitis, abscess).
The most common causes of these complications may be the following:
- result of complications that occurred during the surgery itself,
- ignoring the principles of atraumatic treatment,
- patient's non-compliance with the doctor's prescriptions.
Complications during the reparative regeneration stage
The following complications of the bone regeneration stage are possible:
- mucositis,
- peri-implantitis,
- implant rejection.
Peri-implantitis is a complex of inflammatory phenomena that are localized in the bone tissue surrounding the implant body and are accompanied by bone destruction and filling of the defect area with granulation tissue, which subsequently causes mobility of the implant, and in case of untimely treatment – rejection.
Possible causes of peri-implantitis:
- formation of a hematoma over the cap of the intraosseous component of the implant, followed by its suppuration;
- neglecting recommendations for atraumatic preparation;
- poor isolation of the surgical wound;
- presence of scar changes or a small vestibule of the oral cavity in the patient;
- leaving traumatizing and ischemia-promoting edges near the surgical field;
- unsatisfactory hygiene of the patient;
- lack of carefully established care near the gingival cuff after a one-stage dental implant is placed.
Clinic of peri-implantitis when using one-stage technique
The clinic of peri-implantitis when using the one-stage technique is characterized by the appearance of pain when pressing on the installed implant, the surrounding mucous membrane is swollen, hyperemic, and a slight mobility of the implant is immediately noted.
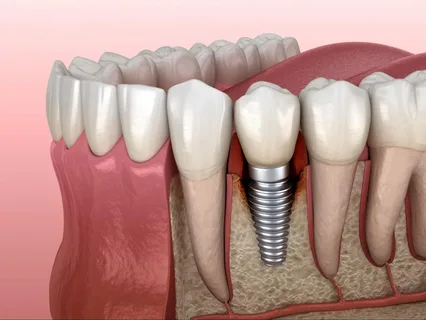
Figure 4. Initial manifestations of resorption at the implant-bone interface.
In the radiograph, an area of bone tissue resorption is clearly defined at the implant/bone boundary, possibly forming a bone pocket localized in the area of the body or neck of the implant.
The principles of treatment involve the following measures:
- conducting professional hygiene, cleaning the protruding elements of the implant in the oral cavity with a scaler to prevent contamination (pollution of the surface of the dental implant, which will create an obstacle to the adsorption of biomolecules, subsequent integration of the implant);
- application of citric acid on the surface of the implant for one minute;
- application of an antibacterial agent to the area of the gingival cuff;
- systemic antibiotic therapy, prescribing metronidazole;
- thorough oral hygiene, antiseptic rinses.
If treatment is unsuccessful, the implant is removed, and the bone wound is revised (atraumatic debridement of granulations). After six months, reimplantation may be conducted.
Clinic of Peri-implantitis with the Use of Two-Stage Technique
Peri-implantitis, developed after the installation of an implant using a two-stage technique, is characterized by a number of features. Several weeks after the surgery, limited hyperemia and swelling form, a fistulous tract or granulations may be noted in the area of the intraosseous element of the dental implant, resembling the clinic of limited osteomyelitis.
On the radiograph, an area of resorption is revealed, which spreads along the implant/bone boundary, beginning to form a bone pocket.
Mucositis is a complex of inflammatory phenomena of the mucous membrane in the area of the screw-cap without joining resorption, or slightly expressed marginal resorption around the neck of the implant.
The most common causes of mucositis:
- penetration of blood into the threaded channel;
- the screw-cap is not securely fixed in the intraosseous element of the implant.
Mucositis can be considered as localized peri-implantitis.
Therapy Principles
Treatment involves the excision of the mucosa over the implant, removal of the plug, treatment of the surgical field and the threaded channel with antiseptic solutions, and placement of the gingival former. All these procedures repeat the algorithm of the second stage of the operation.
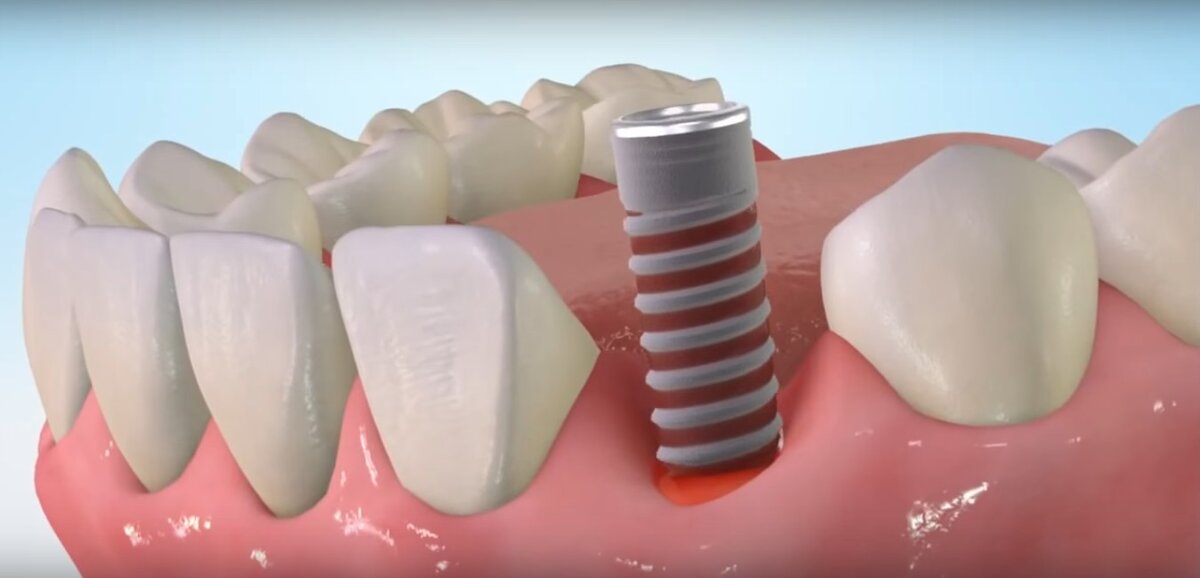
Figure 5. Implant rejection.
If necessary, anti-inflammatory drugs are prescribed. The effectiveness of these measures, provided they are timely, is quite high: inflammatory symptoms disappear within a few days.
Common complications of the second stage of dental implantation:
- unscrewing of the intraosseous fragment along with the cap due to the lack of osseointegration,
- penetration of the intraosseous fragment into the maxillary
sinus, - formation of bone tissue over the cap, which complicates the fitting of superstructures.
According to statistical data, complications of dental implantation, particularly the surgical stage, account for up to 12% provided that atraumatic principles of intervention are followed and high-quality implants that meet modern biotechnical standards are used. The remaining 88-99% are predominantly complications during the orthopedic treatment stage.
Further refinement of techniques and protocols for implantation is associated with the introduction and development of bone tissue regeneration. Membrane technologies, new types of graft materials open up new opportunities for dental implantation.
Learn more about the complications associated with soft tissue augmentation at the webinar Complications of Immediate Implantation.
