Principles of Diagnosis of Benign Neoplasms of the Maxillofacial Area
Machine translation
Original article is written in RU language (link to read it) .
The difficulties in diagnosing benign neoplasms of the maxillofacial area are often due to the variety of forms of the same pathological process, the absence of specific features, and the variability of clinical symptoms against the background of a secondary infection.
For more current information, visit the section of our website Training in Oral and Maxillofacial Surgery.
Today, specialists involved in the diagnosis of benign formations of the dental and maxillofacial system have the following techniques at their disposal:
- collection of clinical data;
- physical diagnostic methods;
- X-ray diagnostics;
- radionuclide diagnostics;
- morphological diagnostics.
Collection of Clinical Data
In the vast majority of cases, benign neoplasms of the bones of the maxillofacial area are characterized by a minimum of clinical symptoms, which is why patients often seek medical attention late. The age and gender of the patient often serve as the starting point in the diagnostic process of neoplasms. This is explained by the fact that precancerous lesions are most often diagnosed in men over 50 years old. For example, in infants, jaw neoplasms and vascular tumors are predominant.
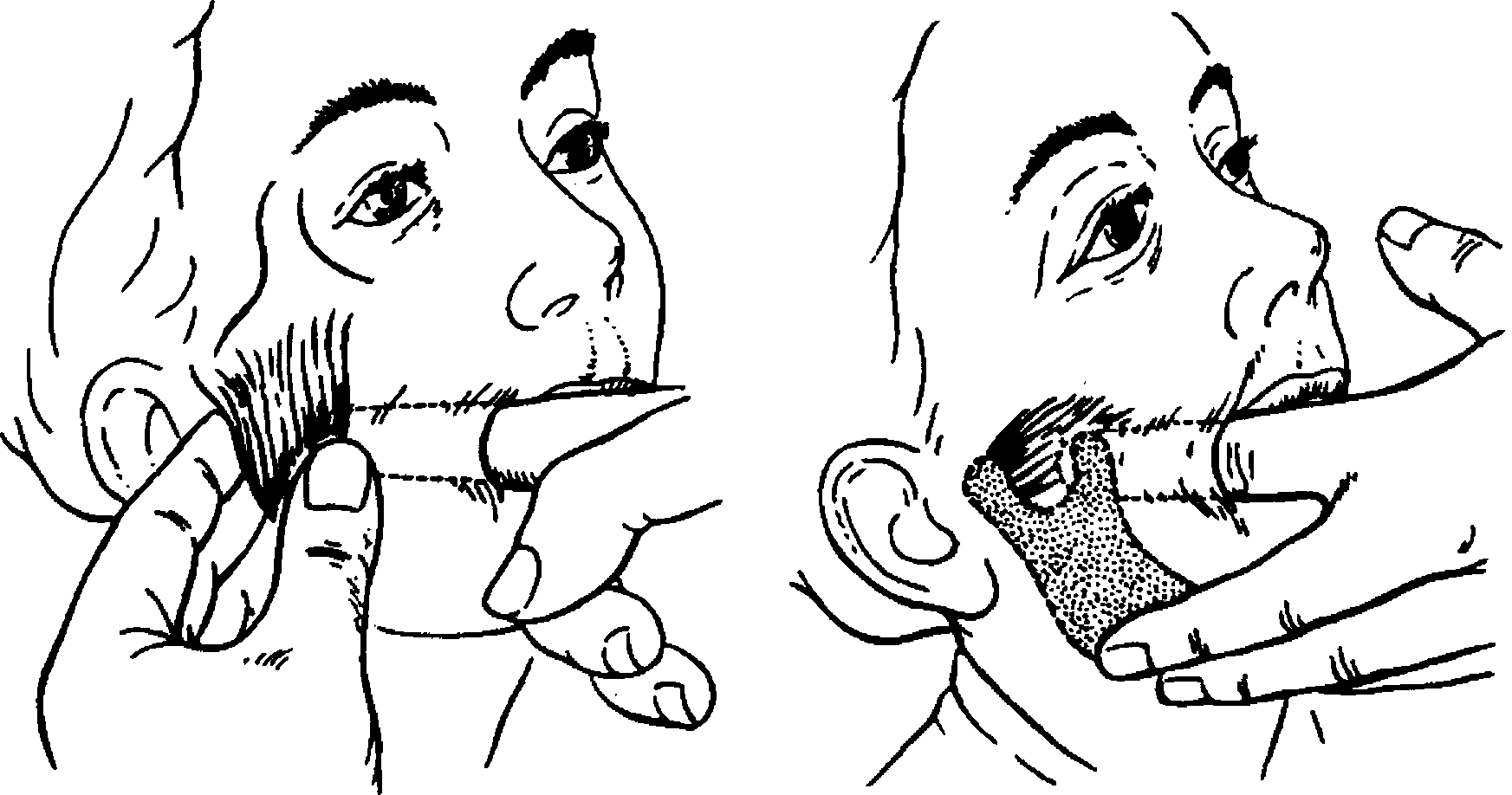
Figure 1. Palpation in dentistry.
Palpation plays a significant role in the diagnostic process. Benign neoplasms typically exhibit expansive growth, characterized by the presence of a well-defined capsule, which can be palpated as a solitary nodule of oval or round shape with clear boundaries. Malignant formations, on the other hand, typically lack a capsule and spread to surrounding tissues, thus they are identified during palpation as a dense infiltrate without clear boundaries.
Jaw formations of the alveolar processes of the jaws are diagnosed early, whereas tumors of the jaw body grow and develop asymptomatically over a long period. The tumor process, when localized in the area of the branch or angle of the lower jaw, and neoplasms of the accessory sinuses are much more difficult to detect.
The compact bone in the area of the branch and angle of the lower jaw predominates over the cancellous bone. Moreover, the bone in this area is covered internally and externally by masticatory muscles – this creates conditions for the late detection of a tumor in this location compared to tumors of the jaw body. The patient's face begins to deform when the pathological process affects more than half of the jaw branch.
Intraosseous neoplasms initially cause damage to the cancellous bone, then lead to thinning of the cortical plate, followed by deformation of the jaw. Thanks to its anatomical position, the lower jaw is completely accessible for examination and palpation, which allows the tumor to be palpated, but at later stages of growth.
A tumor of the bone tissue growing within the body of the jaw can cause such significant thinning of the bone that a pathological fracture occurs. Neoplasms of the upper jaw, its orbital surface, can provoke diplopia and displacement of the eyeball. When the tumor presses on the nasolacrimal duct, tearing is observed.
Tumors that are located on the infratemporal surface of the upper jaw develop absolutely asymptomatically. The initial symptom of such a neoplasm is a feeling of obstruction when opening the mouth wide, which is due to the coronoid process embedding into the tumor. In this case, the patient does not feel pain.
The consequence of the tumor process affecting the frontal process of the upper jaw may result in deformation located at the base of the nose or the inner wall of the orbit, which is often accompanied by symptoms of brain herniation.
Neoplasms of the zygomatic process, extending to the tubercle of the upper jaw, can significantly weaken the strength of the bone. The alveolar process of the upper jaw is a typical area for the occurrence of various benign neoplasms: fibromas, osteoblastoclastomas, osteomas, odontomas.

Figure 2. Palpation of lymph nodes.
Surgical intervention for the removal of a neoplasm on the upper jaw can compromise the integrity of the maxillary sinus, which explains the necessity of preparing a protective plate during the preoperative stage. In the case of surgical intervention in the frontal section of the alveolar process of the upper jaw, the integrity of the nasal cavity may be compromised, subsequently leading to the formation of fistulas that are difficult to treat.
According to scientific literature, benign tumors of the zygomatic bones are rare. When suspecting a neoplasm, special attention should be paid to the areas of regional lymphatic drainage. However, it is important to remember about changes in the lymph nodes, which may be a result of chronic lymphadenitis, caused by inflammatory processes in the maxillofacial area.
Radiological Diagnosis
This represents an auxiliary diagnostic method, used exclusively for pathological processes in the jaws. Today, many special positions have been developed that allow achieving an image of the required fragment of bone tissue in the required projection.
It is easier to determine the radiological signs of a tumor process when it is localized within the lower jaw. Identifying a neoplasm of the upper jaw, and especially of the paranasal sinuses, radiologically is significantly more difficult.
For this reason, when diagnosing a neoplasm of the upper jaw, it is better to use tomography – a technique of layered radiological examination, which allows for multiple imaging of different layers of the tumor.
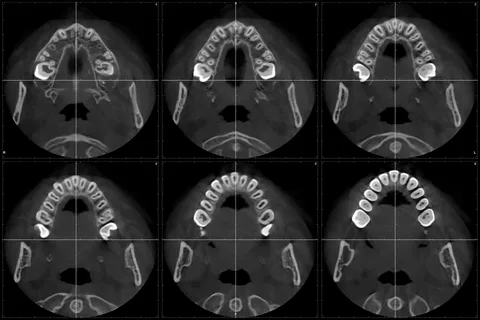
Figure 3. Computed Tomography.
Computed tomography is the most widely used method of X-ray diagnostics today.
Advantages
- High informativeness.
- Allows to obtain images of any tissues.
- Provides images not only of the organ under study but also of the surrounding tissues on the same slice, allowing assessment of their size, configuration, and topographical relationship.
- It is possible to assemble cross-sectional images to create a longitudinal image of the desired fragment.
- Allows to significantly enlarge the pathological focus, perform precise measurements.
- Delivers a clear image regardless of the different densities of tissues.
Physical Diagnostic Methods
Electroodontodiagnosis (EOD) is a widely used method for diagnosing benign jaw tumors, based on assessing the tooth's response to an electrical impulse. The method helps determine the viability of the tooth. EOD is used for diagnosing tumors of the lower jaw and the paranasal sinuses, characterized by disrupted electrical excitability of the teeth.
Morphological Diagnosis
It represents the most reliable method of diagnosing neoplasms.

Figure 4. Fine needle biopsy.
Today, the role of morphological, particularly histological studies, is increasing, which is explained by the introduction of modern biopsy methods and the variety of surgical interventions. Detailed histological characterization of the pathological focus allows for an accurate diagnosis, justifies the chosen treatment strategy, and plans the extent of the upcoming surgical intervention.
Performing a biopsy dynamically helps to monitor the effectiveness of the chosen treatment. A biopsy involves the microscopic examination of a tissue sample taken from a living body for the purposes of diagnosis and treatment planning. The following specimens are subjected to microscopic examination:
- tissue pieces that were removed during surgical intervention;
- aspirates;
- scrapings;
- excreta;
- secretions.
Types of biopsies most commonly used in the diagnosis of benign neoplasms of the maxillofacial area:
- excisional,
- incisional, puncture,
- trepanobiopsy,
- cytological examination of smears-imprints, scrapings, aspirates, secretions, and excreta.
The histogenesis of benign neoplasms is diverse, but they typically share common features:
- slow growth,
- absence of metastasis;
- growth cessation in some cases;
- involutional changes.
Benign tumors are characterized by expansive growth, which results in well-defined contours, making these formations operable.
Some types of benign neoplasms (fibroma, hemangioma) exhibit diffuse infiltrative growth, invade surrounding tissues, and are capable of recurring like malignant processes.
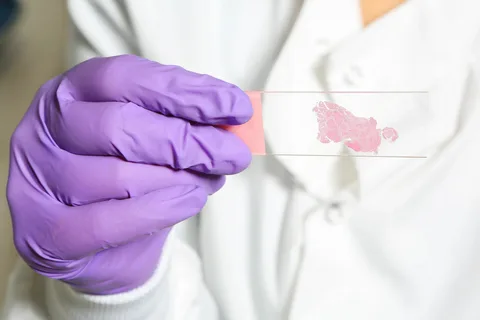
Figure 5. Smear-imprint.
Large benign tumors (osteoma, fibroma, lipoma) can compress and displace adjacent organs, provoking endocrine disorders. For this reason, benignity is a relative concept.
More about the necessity of computer tomography in treatment planning at the webinar CBCT and its impact on treatment planning and decision making.
