Chronic pulpitis
Machine translation
Original article is written in RU language (link to read it) .
Chronic pulpitis – is a chronic inflammation of the tooth pulp. It can be a result of acute inflammation (acute pulpitis) or develop independently. Many factors influence whether the inflammation will initially be acute or chronic. These include one's own immunity, capable or incapable of a vigorous response to the irritant, and the properties of the irritant itself: its strength and duration of exposure.
For more relevant information on this topic, attend the webinar Pulpitis and Apical Periodontitis of Permanent Teeth with Incomplete Root Formation.
The causes of chronic pulpitis can be numerous:
- caries (the most common). It is known that the pulp reacts even to a shallow carious cavity. However, these changes can only be detected at the microscopic level. And if the cavity is deep – microorganisms along with their toxins can penetrate through the dentinal tubules and dentinal fluid into the pulp chamber, ultimately causing inflammation of the pulp.

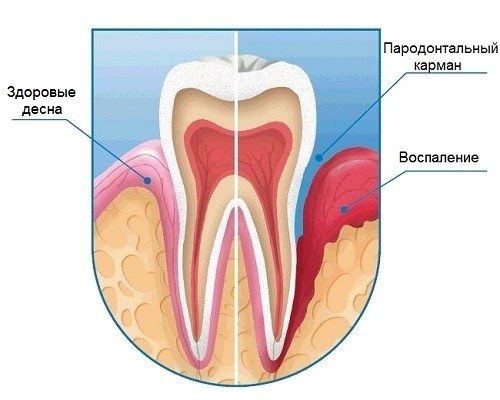
- diseases of the marginal periodontium. In these diseases, the tooth-gingival attachment is destroyed. As a result, microorganisms from dental plaque have the opportunity to settle on the tooth root. From there, they can directly reach the pulp through the lateral canals or the apical opening.
- trauma. Acute – for acute, chronic – for chronic pulpitis. Chronic tooth trauma – most often it is due to overloading. It occurs due to improper bite, an elevated filling, orthodontic appliances. In response to such impact, various pathological changes can occur in the pulp, including chronic inflammation.

- iatrogenic factors. It is no secret that different stages of dental treatment can provoke such a response from the pulp. During preparation – it's overheating, vibrations, accidental opening of the pulp chamber. When filling with modern composites – violation of the etching regime, adhesive techniques, exposure to the light of a polymerization lamp. Conducting professional hygiene, for example, using high-frequency ultrasound, can also cause inflammation of the tooth pulp.
- idiopathic (unclear) causes. When there is no visible local reason for the development of pulpitis.
Clinic of Chronic Pulpitis
Chronic inflammation of the pulp differs from acute by the appearance of a third phase of inflammation – proliferation. Thanks to this stage, the inflammation is localized, and its intensity decreases. Because of this, the clinic of chronic pulpitis has its own characteristics:
- the process is very prolonged, it can take from several weeks to several years;
- pain in response to irritants is mild. And it does not differ much from that in deep caries. And if the cavity – the cause of the pulpitis – is located in some hard-to-reach place (for example, on the approximal surface), then the patient may not be bothered at all. Various factors provoke pain, depending on the form of chronic pulpitis.
Chronic Forms of Pulpitis
There are several chronic forms of pulpitis. And, as often happens, their names differ in different classifications. The most commonly used classifications of chronic pulpitis are ICD-10 and E.M. Gofung.
Chronic pulpitis according to Gofung:
Chronic pulpitis:
- simple;
- hypertrophic;
- gangrenous.
Chronic pulpitis according to ICD-10:
- K04. Diseases of pulp and periapical tissues.
- K04.0. Pulpitis.
- K04.03. Chronic pulpitis.
- K04.04. Chronic ulcerative pulpitis.
- K04.05. Chronic hyperplastic pulpitis.
- K04.1. Pulp necrosis.
These names correspond simply, except for chronic ulcerative pulpitis (ICD-10). There is no equivalent for it in Gofung's classification.
| Gofung | ICD-10 |
| simple | chronic pulpitis |
| hypertrophic | chronic hyperplastic pulpitis |
| gangrenous | pulp necrosis |
It is also possible to encounter such a name for chronic (simple) pulpitis as "chronic fibrous" (by analogy with chronic fibrous periodontitis). This name originally appeared in the classification of KMI (Kiev Medical University) and is still used in the literature.
To more conveniently describe each form of chronic pulpitis, one can use the following scheme:
Results of the main research methods:
- Interview
- Examination
- Probing
- Percussion
- Palpation
Results of additional research methods:
- Electroodontodiagnosis (EOD)
- X-ray
Chronic Fibrous Pulpitis
Chronic fibrous pulpitis, also known as chronic simple/chronic pulpitis:
Interview
During the interview, it is found that our patient is bothered by tooth pain. Its description:
- occurs in response to irritants – temperature (too cold or hot, sudden change in external temperature), chemical (sweet), mechanical (from food, toothpicks);
- aching, does not subside long after the cause of the pain has ceased.

According to such symptoms, another test can be conducted – a thermal test. The reaction to it will be positive in the case of chronic simple pulpitis.
But! There might be no pain at all, then it is referred to as an asymptomatic course of pulpitis.
Also, our patient may mention that the tooth had been painful before. The cause of the pain could have been caries, which led to the inflammation of the pulp. Or an acute pulpitis that turned into a chronic form.
Examination
Of course, the patient's appearance does not raise any concerns. Only the affected tooth draws attention, specifically a deep carious cavity in it (if pulpitis is a complication of caries), which may also be under a filling. The tooth cavity is usually not opened. However, if it is opened during preparation, the inflamed pulp bleeds and hurts.


Probing
The bottom of the carious cavity is painful at one point – the projection of the closest part of the pulp. Difference from deep caries: there, the entire bottom is sensitive, all its peripulpal dentin.
- Percussion is painless.
- Palpation of the transitional fold in the area of the tooth root apex is also painless.
There are no reasons for pain during percussion and palpation: the inflammation is only in the tooth cavity. The surrounding tissues are not involved (yet).
- EOD – 40-60 microamperes. But it can give a false result, indicators of the norm (2-6 µA).
- X-ray – carious cavity, if it is the cause of the pulp inflammation. No changes in the periapical tissues. However, with increased reactivity of the body, for example, expansion of the periodontal gap may occur.
Chronic Ulcerative Pulpitis
Chronic ulcerative pulpitis is very similar to chronic simple pulpitis. Common are complaints, results of additional examinations, percussion, and palpation. However, there are differences (upon examination and probing):
Unlike chronic simple pulpitis
- there is communication with the tooth cavity;
- the pulp at the site of communication has a characteristic appearance: ulcerative surface, may be covered with a layer of necrotic plaque;
- the reaction to probing is painful or mildly painful, the pulp bleeds.

Chronic Hypertrophic Pulpitis
Chronic hypertrophic pulpitis, also known as chronic hyperplastic pulpitis (ICD), most often develops if the tooth crown is severely destroyed + the cervical margin of the tooth is one of the walls of the carious cavity. This creates conditions for the inflamed hypertrophied pulp to grow into it. Young age is also an important, but not primary condition. The fact is that the likelihood of such active proliferation of pulp elements is higher, the higher the reactivity of the organism.

Survey
In addition to complaints of aching pain, as with chronic simple pulpitis, there are several more:
- growth of "wild meat" in the tooth or in its place;
- its bleeding, pain, especially when eating, when it is injured by antagonist teeth and food.
Examination
We see a carious cavity, filled to a greater or lesser extent with soft tissue. Its color and consistency may vary depending on the degree of its maturation. Young tissue will be bright pink, even red, soft, similar to granulation tissue. More mature tissue, the so-called "pulp polyp," is tumor-like, pale pink, dense.

Probing
Varies for the same reason. Immature tissue easily bleeds, painful. Probing of formed tissue does not lead to bleeding, slightly painful.
Percussion, palpation are painless.
- EOD – 20-40 µA.
- X-ray – no changes.
Another distinctive feature of this chronic pulpitis is a negative thermal test: the tooth does not react to temperature stimuli.
Chronic Gangrenous Pulpitis
Chronic gangrenous pulpitis (pulp necrosis) is the death of pulp cells. This outcome can be caused by inflammation or trauma.
Survey
Our patient is troubled by aching pains from various irritants. He is exhausted, as after the removal of these irritants, the pain does not subside or subsides slowly. The pain is especially pronounced in response to heat. It hurts from hot tea, and from a sharp change in temperature (for example, entering a warm apartment from a frosty street). He can recall that it hurt more in the past. Some "lucky ones" may not be bothered by pain at all. Or there might be another complaint – an unpleasant smell from the mouth.
Patients may also be concerned about a changed tooth color. This is especially relevant if the causative tooth is located in the frontal section. The enamel of a tooth with pulp necrosis turns gray. This complaint may even be the only one if the pulp death occurred as a result of trauma. Asking about it during the survey would be far from superfluous.

Examination
The naked eye can see the gray color of the tooth enamel, the deep carious cavity, and the large communication with the tooth cavity. The pulp is dirty, dark, mushy, with a foul smell. In the crown part, it may completely disintegrate.
In the case of pulpitis from trauma, the tooth looks intact, only betrayed by a darker color of the enamel. The pulp in such a case appears as a dry strand, not a shapeless mass. This is because the cause of its death is not microorganisms and their toxins, but a disruption of blood circulation.
Probing
The pulp necrotizes, and along with it, the nerve endings die. Only in the distant sections of the pulp (its orifice or in the root canals) does sensitivity and bleeding remain.
This feature of probing helps to distinguish pulp necrosis from other similar conditions. For example:
- the pulp in chronic ulcerative pulpitis has a similar appearance. However, its sensitivity is still preserved in the crown part;
- quite different – chronic apical periodontitis. In such a tooth, there is nothing left of the pulp, any endodontic instrument will not cause any unpleasant sensations.
- Percussion – can already be painful, very close to periodontitis.
- Palpation of the mucobuccal fold – still painless.
- EPT – up to 90 µA (almost complete pulp breakdown).
- X-ray: possible widening of the periodontal ligament space, bone destruction in the apex area, if the infection has already affected the adjacent periapical tissues besides the pulp.

Exacerbation of Chronic Pulpitis
The clinical presentation of an exacerbation of chronic pulpitis is the same as in an acute condition, acute pulpitis. The exception is the information that the patient can provide. About how the tooth has been troubling for a long time, already hurt before as it hurts now. Or report some factor that could have triggered the exacerbation of a chronic process (hypothermia or a photofill in a tooth where pulp inflammation was not suspected). 
About the principles of anesthesia in the treatment of pulpitis at the webinar Managing the Pain Component in Pulpitis.

