Features of Prostheses Supported by Endosteal Implants
Machine translation
Original article is written in RU language (link to read it) .
The key difference between a tooth and an implant, which must be considered during orthopedic treatment, lies in the complete immobility of the osseointegrated implant, whereas a tooth exhibits some physiological mobility, approximately 100 microns.
Learn more about the risks of prosthetics on implants in the webinar Occlusion of Prostheses on Implants. Biomechanics.
Normally, healthy periodontal fibers of a tooth provide cushioning of masticatory pressure, its partial redistribution to the walls of the bone socket, the jawbone, and adjacent teeth.
The dental endosteal implant, which is inserted into the thickness of the bone tissue of the alveolar ridge, is a foreign body, however, due to the bioinert properties of titanium, the material from which implants are made, there is no rejection. In the postoperative period, the implant is covered with bone, forming a physiological ankylosis. Masticatory pressure is transmitted directly from the implant to the bone, as there are no periodontal fibers to provide cushioning.

Figure 1. Bridge prosthesis on implants.
An osseointegrated implant does not possess physiological mobility. However, this does not prevent it from functioning successfully either alone or in conjunction with other implants.
An unfavorable situation for the implant arises if it serves as one of the supports of a bridge prosthesis, while a natural tooth serves as the other support. In this case, the chewing load exerted on the tooth is not cushioned by the periodontium, as the tooth lacks physiological mobility, and it is fully transferred to the implant. Constant overload of the implant leads to deterioration of the osseointegrative connection, provokes peri-implantitis, which may result in the removal of the implant in the future.
Ideally, the restoration of dental integrity should be performed exclusively with crowns that are supported by implants, without using the patient's remaining teeth as supports.
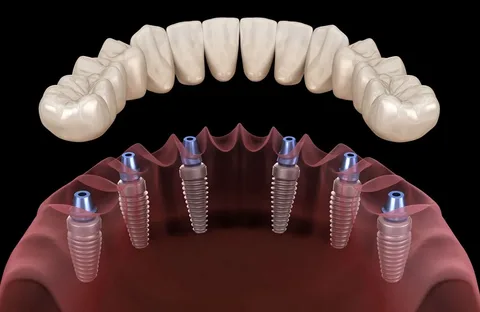
Figure 2. Prosthetics of an edentulous jaw on implants.
If the clinical situation requires the installation of a bridge prosthesis, where both implants and the patient's own teeth will be used as supports, it is necessary to splint the teeth, which will reduce the physiological mobility of these teeth and significantly lower the risk of overload. The likelihood of overload also decreases if implants are used in the bridge prosthesis as an intermediate support in cases of extensive defects in the dental arch.
Types of Constructions That Prevent Implant Overload
Special types of constructions have been developed that are used to prevent implant overload. The following types are distinguished:
- crushers,
- load dampers.
These constructions consist of semi-labile locking attachments or detachable connecting devices with locking or screw fixation, which combine the components of a non-removable prosthesis, ensuring slight mobility of one of the parts.

Figure 3. Implant osseointegration.
The technique of creating a prosthesis with load breakers is quite complex, requiring the use of expensive equipment.
Conditionally removable structures can provide a similar function thanks to their threaded connection, which allows maintaining a slight mobility of the non-removable prosthesis installed on the implant. This significantly minimizes the likelihood of implant overload. The chewing load is transferred along the axis of the implant, reducing the risk of overload. The chewing pressure is redistributed to the surrounding bone, protecting the alveolar ridge from atrophy.
Previously, the use of dental screw implants involved their submucosal implantation, which was considered an essential condition for successful osseointegration. This period was three months for the lower jaw and six months for the upper jaw. Subsequently, the implantation technique involved exposing the implant, removing the plug, and screwing in the gingival former. A week later, direct prosthetization could begin.
As implantology has developed, the techniques and time for implant integration have undergone significant changes. Techniques for immediate loading of implants appeared, many specialists believed that they contributed to the accelerated formation of bone tissue around the implant under constant physiological load. However, it is important to consider that the load should not be traumatic, so as not to damage the primary stability of the structure. Immediate loading was performed using non-removable provisional prostheses. Osseointegration of implants occurred after 3-6 months, after which it was possible to proceed with permanent prosthetics.
Outcomes of implantation determined by the load on the implant
The following situations are possible during implantation:
- the implant is placed under the mucoperiosteal flap;
- it is unloaded;
- it is freely loaded;
- it is splinted.
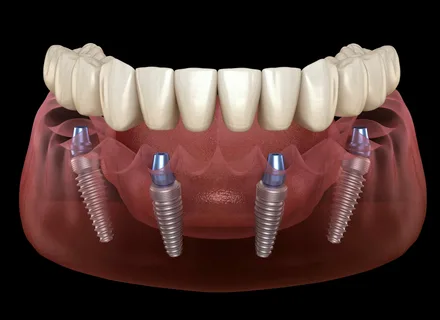
Figure 4. Removable denture on four implants.
1st case. The load on the implant is applied after 3-4 months. During this period, the patient uses a removable provisional denture.
2nd case. Above the mucous membrane, there is a platform with a screw or thread for denture fixation, the implant itself is not subjected to load, therefore there are no indications for installing temporary structures.
3rd case. Three weeks after implantation, it is recommended to manufacture permanent dentures, which will provide splinting and chewing. There is no need for temporary dentures.
4th case provisional dentures are made on the eve of dental implantation, and they are fixed immediately after the implants are installed.
Features of temporary dentures
- their manufacture depends on the specific clinical situation;
- used to fix the height of the bite;
- help minimize implant mobility;
- used for aesthetic reasons.
During the planning of a future prosthesis construction, it is important to remember about arch stabilization or parasagittal stabilization, and to ensure that the chewing pressure is transmitted to the implant exclusively vertically, which will help reduce the risk of implant migration.
- Chewing pressure, when overloading the implant, becomes a traumatic factor that provokes disruption of osseointegration. For this reason, during the modeling of the chewing surface of the crown, it is important to observe the following conditions:
- The occlusal surface should have several contacts in the position of central occlusion, distributed across different cusps.
- It is important that the area of the occlusal surface is narrower than the area of the occlusal surface of the crown that rests on the tooth (not more than the area of the occlusal surface of a premolar).
- The chewing surface of orthopedic constructions must exclude supracontacts in any phase of articulation.
- Do not use cantilever constructions that rely on implants, except for "distal extension" in the presence of an edentulous jaw, when the bridge-like prosthesis is supported by 5-6 implants with arch stabilization.
During the fabrication of a fixed prosthesis, the occlusal surface of the crowns is modeled to be one-third smaller than the area of the patient's own teeth with a weakly pronounced equator. In a bridge prosthesis, the intermediate part is made bullet-shaped or heart-shaped. It is important not to create pronounced grooves and bumps on the occlusal surface to prevent high loads, inflammation of the mucous membrane under the prosthesis body, and to prevent loosening loads due to the blocking of jaw function.
The gingival zone of the intermediate part is modeled to optimize hygiene care. In implantology, the most optimal design is a combined occlusal surface, where only the occlusal plates in the areas of vertical load on the implant are modeled with metal. Such designs help maintain the height of the bite and improve the grinding of the occlusal surfaces of the teeth.
The technical complexity and volume of work, which determine the final cost, the wear resistance, and high aesthetics of modern composite veneering materials have led to their widespread use in implant prosthetics.
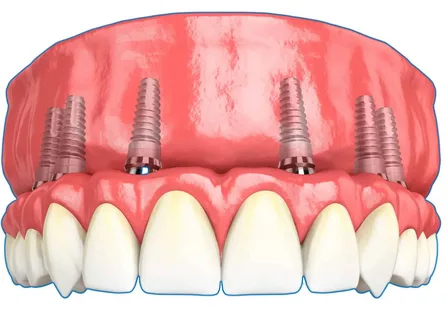
Figure 5. Fixing the prosthesis on implants.
Before fixing a non-removable prosthesis, it is important to ensure the quality of its polishing, which is necessary for self-cleaning and maintaining a high level of individual hygiene. Most specialists recommend fixing prostheses with provisional cements on implants, as these materials allow the structure to be removed without compromising its integrity in case of various complications or for professional hygiene procedures.
More detailed information on this topic is presented in the webinar Digital model of a hybrid prosthesis supported by implants (ALL-ON-4®). Part 1.
