Targeted Tissue Regeneration
Machine translation
Original article is written in RU language (link to read it) .
The technique of guided tissue regeneration was first applied during a flap surgery in 1982 by specialists under the leadership of S. Nyman. To prevent the cementum from adhering to the cells of the gingival flap in the area of the exposed root section, and to prevent the growth of epithelial cells, a Millipore filter was used. This filter was placed between the root surface and the mucoperiosteal flap, which provided the prerequisites for the reconstruction of the periodontal ligament.
Biological principles of guided bone regeneration and types of membranes used are discussed in the webinar Resorbable Membranes in Guided Bone Regeneration.
The dentogingival attachment can be recreated exclusively from periodontal tissues since they are capable of transforming into cementoblasts and inhibiting the growth of other tissues. If this condition is not met, gingival tissues begin to grow, leading to the destruction of the root cementum. The dentogingival junction can also form as bone ankylosis due to the presence of osteoblast precursors in the periodontal ligament tissues – these are cells that can differentiate into cementoblasts and osteoblasts, forming layers of cementum on the root surface, thereby directly participating in the reorganization of the dentogingival junction.

Figure 1. Osteoplastic material is poured under the membrane.
Cell proliferation of the regenerating periodontal ligament occurs between the cement surface and the inner side of the membrane. Thanks to experiments conducted by Nyman's team, a completely new membrane material based on polytetrafluoroethylene and "Millipore" was proposed. This material was later named "Gore-Tex".
Membranes were produced in various configurations, which allowed achieving a high level of fixation in the cervical areas of the teeth. The main drawback of the material is its inability to be absorbed, which explains the need for a subsequent surgical intervention aimed now at removing the membrane.
Since the onset of regeneration occurs approximately 5-6 weeks later, a repeat surgical intervention is planned after this period.
Biodegradable membranes made from resorbable material. Their production is based on the use of glycogenic and lactate polymers, they do not contain plasticizers, and during hydrolysis they decompose into glycolic and lactic acids. Their composition includes collagen, which accelerates the destruction of platelet plaques, stimulates the formation of adhesion in blood clots. Exogenous collagen promotes the activation of fibroblast chemotaxis, accelerates the formation of fibrillar spatial structures around them.
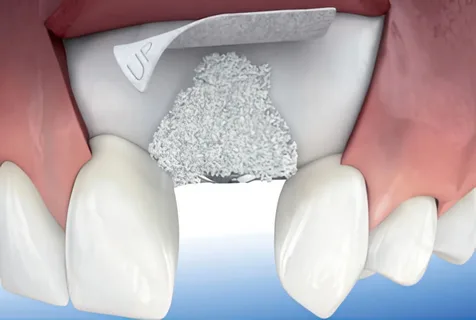
Figure 2. Membrane placement.
If a collagen membrane and a material containing bone additive are combined in a single complex, it will lead to the formation of not only a connective-
tissue structure, but also young bone tissue, which will fill more than half of the original defect. Such membranes are absorbed within a month, and their crown area within a week and a half. This rapid absorption is due to the action of tissue enzymes. To prevent this phenomenon, dual-layer membranes have been developed, in which collagen serves as the outer layer, and the inner lining contains the following additives:
- heparin sulfate;
- growth factor 1;
- fibrin, which activates the proliferation of cells involved in the reconstruction of the periodontal ligament.
Types of Membranes
The variety of membranes can be divided into two groups:
- non-resorbable,
- resorbable.
A representative of the first group is GORETEX – a polytetrafluoroethylene material. Its structure is characterized by pores, the size of which is about 1 micron, allowing the ingrowth of connective tissue, which prevents epithelium from growing along the root surface.
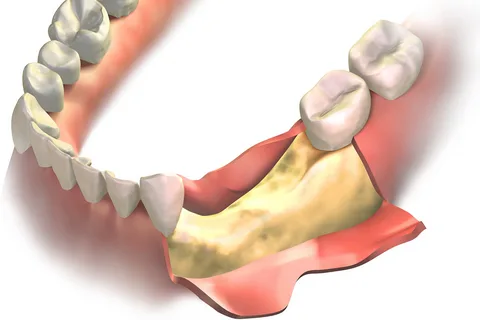
Figure 3. The mucoperiosteal flap is detached.
All modern membranes, to stimulate the formation of organotypic regeneration of periodontal tissues, are released in the form of multi-layered plates. Thanks to morphometric and clinicohistological studies, barriers have been developed that promote the reorganization of the tooth's supporting apparatus and have a predictable treatment effect.
A representative of resorbable membranes is the RESOLUT material, based on a combination of glycogenic and lactate polymers, with the expected therapeutic effect achieved within 1 to 1.5 months.
The list of materials used as separation membranes is diverse. Oxidized cellulose is popular for covering furcation and interdental defects, the material is not released in the form of a membrane, but is a homogeneous mass. After the cellulose comes into contact with a bloody surface, the mass becomes gelatin-like, then gradually dissolves, leaving no toxic products behind.
Another popular material is collagen-like cartilage membranes, which are produced from the cecum of cattle, then chromed, and besides periodontology, are also used as suture material. The dissolution of such membranes is observed over 1-2 months, their structure does not allow the ingrowth of epithelial cells.

Figure 4. Example of a membrane.
The use of membranes made from biodegradable polyester in surgical periodontology practice has allowed for the restoration of the tooth-gingival connection within 4 weeks after surgery, and young bone tissue forms after another 4 weeks. The use of this material has enabled complete filling of furcation defects.
Polyglactin 910 membranes, based on a vicryl mass formed by lactide and glycolide, with a mass ratio of 1:9. The material is synthetically produced. Soft tissue regenerates four times more effectively than in the control group. Inter-root defects are significantly reduced. The introduction of additional artificial bone additives significantly accelerates bone regeneration.
To increase the effectiveness of surgical periodontal treatment of periodontal diseases, a superelastic fabric based on nickel-titanium was proposed as a material for membrane technology. The tissue implant is made from the finest nickel-titanium wire, with a cross-section not exceeding 50-60 µm, and a tissue cell size of 10-100 µm.
Advantages of the material
- characterized by superelasticity,
- excellent biochemical compatibility with surrounding tissues,
- high biomechanical properties.
Using surgical scissors, a piece of membrane necessary for the specific clinical scenario is intraoperatively cut from the tissue implant, considering the topography and size of the bone defect. The feature of the material is that the membrane has a porous open microstructure, into which connective tissue grows, securely fixing itself. Thus, on one hand, it creates a barrier to the growth of epithelium, and on the other hand, it prevents it from sliding along, forming a pocket over the membrane. These membranes have proven very effective in complex clinical cases, where there is a high likelihood of the membrane slipping into the defect. Manufacturers recommend using a membrane based on nickel-titanium to ensure the reconstruction of extensive bone defects.
Usage Technique
A mucoperiosteal flap is created to access the bone defect, it must be tailored so that it completely covers the surface of the membrane over the bone defect without any tension. The membrane should be modeled with an excess so that its edges overlap the bone defect by 4-5 mm. To achieve stability of the submembrane space, the edges of the membrane are tucked under the periosteum.

Figure 5. Collagen-based membrane.
Thanks to the microporosity of the material and the roughness of its surface, the membrane is reliably stabilized over the defect, as is the flap over it. There is no need to additionally fix the membrane to the edge of the bone. To prevent the synthetic tissue membrane from shifting into the bone defect, the space under the membrane is filled with various osteoplastic materials.
Once all layers are placed, the mucoperiosteal flap is repositioned, and then sutured with interrupted or mattress stitches. It is advisable to choose a suture material of the same type – a thread made of nickel-titanium alloy. Sutures are removed after two weeks.
Postoperative care includes frequent rinsing of the oral cavity with antiseptic solutions and avoiding irritating and hard foods.
More detailed information on this topic is available in the online course Directed Regeneration and Navigation Implantation.
