Myofascial Pain Syndrome in TMJ Dysfunction
Machine translation
Original article is written in RU language (link to read it) .
Myofascial pain syndrome can develop in a patient even against the background of an undamaged temporomandibular joint. This pathological condition is a result of fatigue, muscle tension, and less commonly, spasm of the masticatory muscles.
Learn more about this topic at the webinar Splints for treating myofascial problems. Myorelaxing splints.
Trigger Points
Before discussing the clinic of myofascial pain syndrome, it is necessary to consider the concept of trigger points. The key factor contributing to the formation of neuromuscular dysfunction is hyperirritability, which is localized at a strictly defined area – a trigger point. This hyperirritability is due to the sensitization of sensitive nerve endings of a specific muscle.
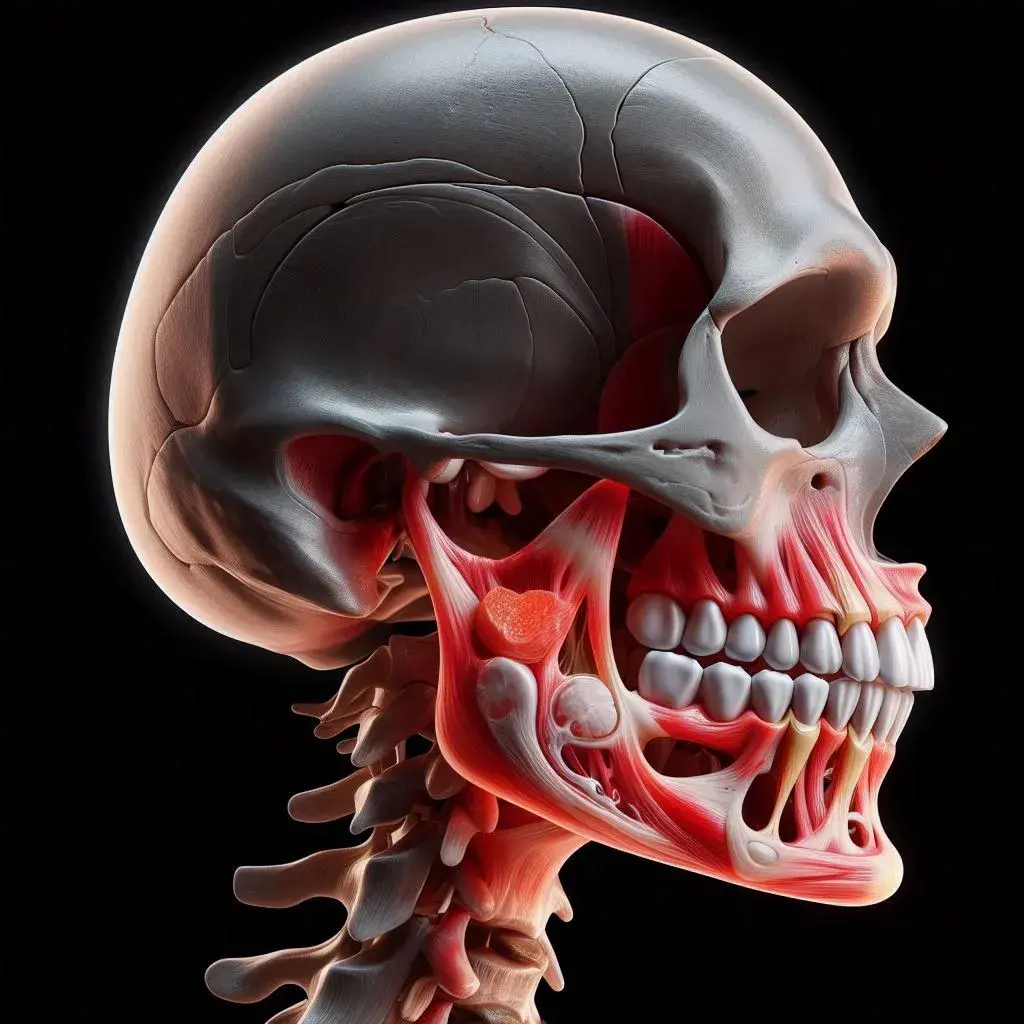
Figure 1. Lower jaw and temporomandibular joint.
Various active biological substances act as sensitizing agents:
serotonin,
histamine,
prostaglandins.
Often, pressor therapy, which stimulates increased blood flow, helps to wash out sensitizing agents from muscle fibers.
Pathogenesis
Local changes occurring in trigger points proceed in the following sequence:
disruption of fat metabolism,
spasm of small vessels, weakening of the strength and activity of local blood flow, slowing of venous outflow,
local accumulation of metabolic products, which can independently cause sensitization of sensitive nerve endings,
muscle fiber tension causes overload of contractile elements, tissues are damaged, as a result, calcium ions leave the sarcoplasmic reticulum,
excess calcium, against the background of energy influx from ATP, maintains constant contracture of muscles affected by the pathological process,
as a result of the listed processes, persistent dystrophic phenomena gradually develop in the muscle, which over time becomes impossible to eliminate.

Figure 2. Pain in myofascial pain syndrome.
Clinical Picture
Characteristic clinical manifestations of myofascial pain syndrome dysfunction TMJD:
The patient complains of sudden onset of sharp pain, difficulty opening the mouth.
In some patients, the appearance of pain is preceded by clicking in the joint over a long period, excessive or limited mobility of the jaw, and other symptoms of TMJD dysfunction may be present.
The clinic can be divided into several periods: dysfunction and painful contracture of the masticatory muscles, often accompanied by limited mouth opening.
The pathological process can begin with any of these periods, determined by the intensity and type of irritant affecting the masticatory muscles, and the patient's psycho-emotional state.
During emotional stress, spontaneous, often prolonged contraction of muscle fibers occurs, accompanied by pain.
In most cases, pain appears sharply after waking up, when eating hard food, physical exhaustion, excessive mouth opening.
The pain is dull, prolonged, occurring both at rest and during movements of the lower jaw.
The patient's intensity of pain sensations can vary from slight discomfort to excruciating sharp attacks of pain.
Palpation reveals a painful, clearly localized dense fragment of the muscle – a trigger point, pressing on which with a finger increases the pain and radiates to different parts of the face.
Pain occurring after sleep is explained by bruxism. Pain that occurs during the day is due to the patient's psycho-emotional state, the presence of a predisposition to reflex muscle fiber spasm against the background of their overload or hypothermia.
The development of spasm provokes pain sensations in the muscle, causing movement disorders in the joint.
The joint itself can also be a source of pain.
The aching, unceasing pain symptomatology has various localizations: in the masticatory or temporal muscles, behind the upper jaw tubercle; pain radiation is also different: neck, forehead, orbits, shoulder, forearm.
The enhancement of dull, unceasing pain in patients is caused by any movements of the lower jaw: when chewing hard food, needing to shift the jaw to the side, when attempting to open the mouth wide.
Stress is the most common catalyst for pain.
In response to stress, muscles often respond with a spasm or a decrease in tone, the emergence of tension, and the formation of trigger zones in the muscles. A trigger point, localized in the masticatory muscle, can mimic tooth hypersensitivity to temperature irritants, percussion.
Trigger Points in Myofascial Pain Syndrome
When a trigger point is located in the medial pterygoid muscle, pain irradiation is observed in the tongue, throat, palate, retromolar area, and the base of the nose.

Figure 3. Pain irradiation when the trigger point is located in the temporal muscle area.
If the trigger point is located in the temporal muscle, the patient often complains of headaches. Pain sensations may occur in the teeth of the upper jaw due to increased sensitivity to temperature fluctuations, typical pain during percussion, and limited mouth opening. When the trigger zone is predominantly located in the anterior part of the temporal muscle, reflected pain is typical in the incisors of the upper jaw and along the upper edge of the orbit; if located in the middle part – pain sensations appear locally and are reflected in the molar teeth of the upper jaw, or in the temporomandibular joint. If the trigger point is located in the posterior part of the muscle, pain is noted at that site.
Trigger points of the masticatory muscle, their location and symptomatic features:
Anterior edge of the muscle, upper part – characteristic pain in the molar teeth of the upper jaw, infraorbital area.
The lower part of the muscle - pain is reflected in the distal parts of the lower jaw, molars.
Along the lower edge of the muscle - irradiation of pain sensations along the lower jaw.
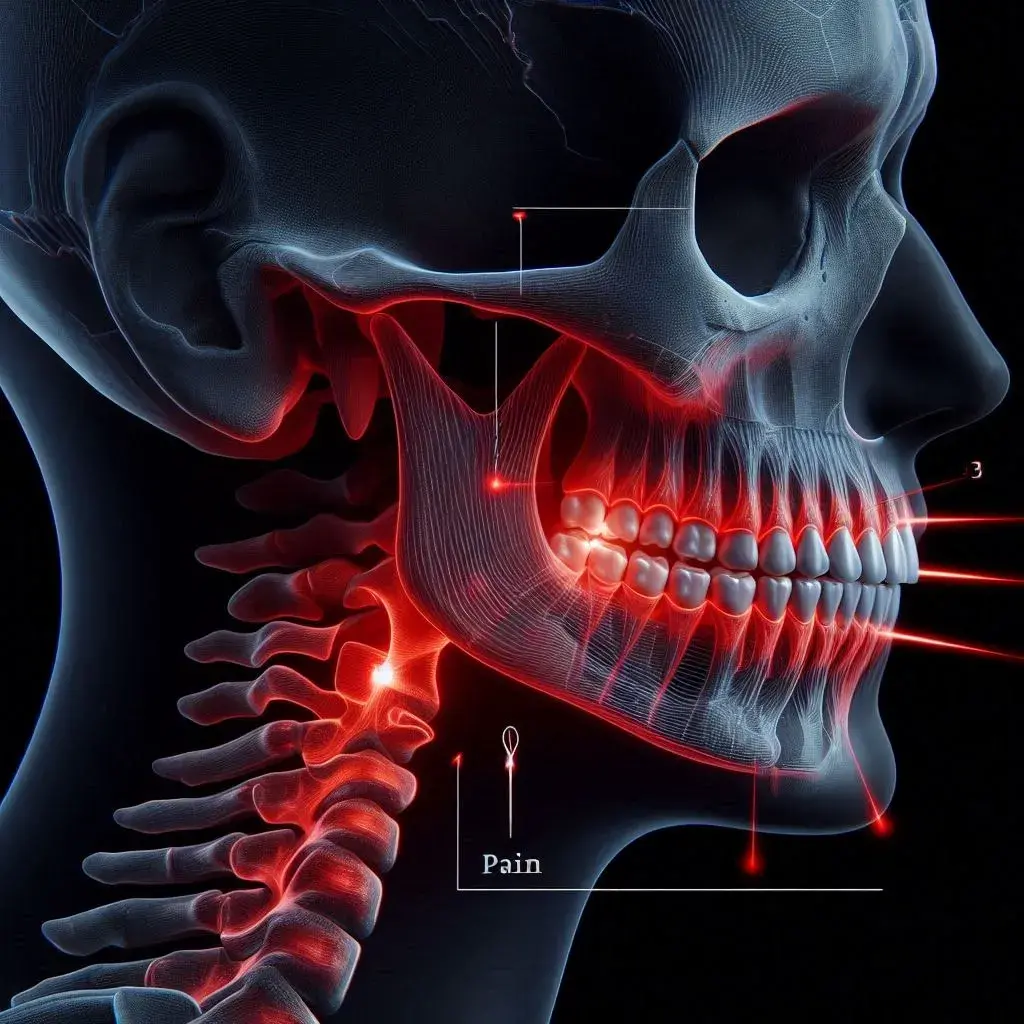
Figure 4. Pain irradiation when a trigger point is located in the area of the masticatory muscle.
If a trigger point is predominantly localized in the superficial layers of the masticatory muscle, the pain is accompanied by jaw clenching, such a symptom is extremely rare when the trigger zone is located in the deep layers of the muscle.
Factors that cause activation of trigger points in muscles:
direct trauma to a specific muscle;
immobilization of the muscle for an extended period of time (in case of a fracture);
the habit of constantly chewing gum;
bruxism;
hypothermia, drafts;
psycho-emotional strain;
lack of multiple firm interdental contacts.
Solving the problem of eliminating the pain syndrome that has been tormenting the patient for a long time is a crucial, but challenging task. The existence of pain trigger points over a long period is explained by the formation of a "vicious circle," where the contraction of a certain muscle causes an increase in pain, and the pain itself contributes to even greater contraction of the masticatory musculature. In such a situation, it is important to break the "vicious circle" as soon as possible.
Treatment Principles
Key measures that should be taken when diagnosing a patient with myofascial pain syndrome against the background of parafunction of the chewing muscles, dysfunction of the temporomandibular joint:
selective grinding, achieving tight interdental contacts;
re-prosthetics;
creation of plastic caps with intact rows;
performing blockades;
treatment of bruxism;
prescription of muscle relaxants, tranquilizers;
elimination or minimization of irritating muscle factors, ensuring maximum muscle rest.
If, despite the measures taken, the patient continues to experience constant aching pain that does not subside after performing a blockade and is not relieved by other therapeutic manipulations, it is possible to assume the development of organic changes in the affected muscle, which are associated with the prolonged existence of a spasm.
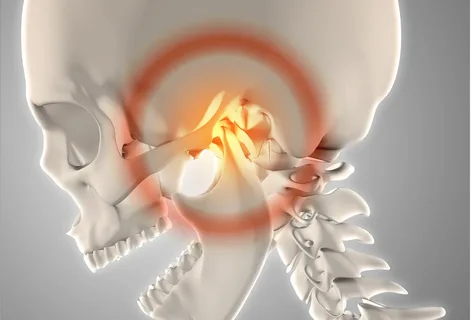
Figure 5. Normalization of the temporomandibular joint.
Against the background of pain sensations in some patients, a decrease in the mobility of the lower jaw is observed simultaneously or over time. Normally, the distance between the incisors is about 45-55 mm, but against the background of pain syndrome, it drops to 5-15 mm. The patient is unable to lower the jaw further due to severe pain. Movements of the lower jaw to the sides and forward are also restricted. In the presence of mild pain or its absence, a patient may experience a sudden clenching of the jaws.
More current information about myofascial pain, causes, diagnosis, and treatment in the webinar on myofascial pain, central myalgia, and fibromyalgia. Module 4Managing Muscle Pain. Part 3. Myofascial Pain, Central Myalgia, and Fibromyalgia. Module 4.
