Fundamentals of Adhesive Dentistry
Machine translation
Original article is written in RU language (link to read it) .
Adhesive dentistry forms the basis that has led to fundamental transformations in aesthetic dentistry – the concept of adhesion for direct composite restorations, in prosthetics – protocols for fixing ceramic products.
About the advantages of adhesive restoration at the webinar Adhesive Dentistry: A Biological Approach to Tooth Treatment and Pulp Vitality Preservation.
However, there remains a whole complex of unresolved problems in adhesive dentistry:
- adhesion to root cement and sclerotic dentin of composite materials,
- sensitivity to moisture of adhesive systems,
- spatial stability against the presence of dentinal fluid, which moves within the system of dentinal tubules,
- the impossibility of restoring periodontal attachment to a defect formed as a result of the carious process on the tooth root.
The ability of a dentist to choose the necessary adhesive system for a specific clinical case confirms his fundamental knowledge, minimizes possible errors that may occur during treatment.

Figure 1. Representatives of adhesive systems.
Adhesive Systems
Adhesive dentistry is the foundation of minimally invasive therapy for the hard tissues of the tooth.
Let's recall what an adhesive system is. It consists of several solutions, the combination of which facilitates the formation of intermolecular interactions at the boundary of heterogeneous structures (tooth tissue/composite), providing a micromechanical connection between these structures. The modification of the latest generations of adhesive systems has simplified the adhesion procedure, combining all components of the system in one bottle – "all-in-one". However, despite the numerous advantages of this solution, using such a modern adhesive system may not always be the right choice in all clinical situations.
Versatility is the main characteristic of an adhesive system that specialists aim for today when developing the latest representatives of adhesives.
The sequence of steps in adhesive preparation:
- etching the surface of tooth tissues;
- applying a primer;
- applying the adhesive.
Types of Etching
As a result of preparation, the enamel prisms are subjected to cutting in several planes: vertically and transversely.
The following types of etching are distinguished:
- Central type, during which the enamel prisms are predominantly dissolved in their central sections: the acid dissolves the core of the prisms, but the shell is preserved.
- Peripheral type, it is characterized by the destruction of the enamel prism shell under the influence of acid, while the core remains. Around the periphery of the enamel prisms, marginal cracks of various sizes and directions are observed, mainly occurring in the head sections of the prisms.
- Low-retention type is characterized by the action of acid on areas free from enamel prisms.
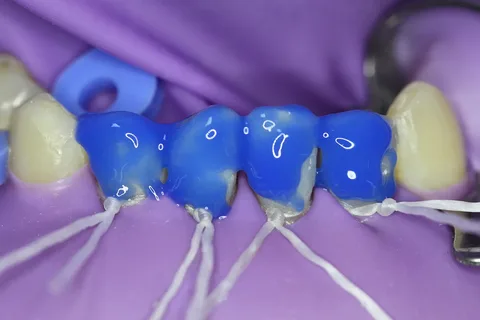
Figure 2. Total etching of enamel.
Characteristics of Etched Surfaces
The surface of the enamel becomes porous after etching, its crystalline structure is loosened, and microscopically the enamel acquires a granulated appearance.
Normally, areas of enamel that lack prisms can only be found in recently erupted teeth or in the cervical regions of teeth in elderly patients. On average, the length of enamel areas free from enamel prisms is about 10-30 mm.
The surface of dentin after etching includes numerous exposed dentinal tubules, due to the dissolution of demineralized dentin and the disappearance of the "smeared" layer under the influence of acid. The latter represents an area on the dentin surface formed as a result of preparation, including denatured collagen fibers, broken fragments of dentinal tubules, hydroxyapatite crystals, saliva components, and bacterial flora.

Figure 3. Etching gels.
The thickness of the smeared layer reaches about 5-10 microns. To adequately etch the dentin, an exposure of 10-20 seconds to the etching agent, which has a pH of 0.5-1.5, is sufficient. The low pH of the applied composition ensures the formation of a strong bond due to the creation of a high-density hybrid
layer.
Demineralization of intra- and peritubular dentin creates the conditions for the dentinal tubules to expand, hydroxyapatite crystals to dissolve up to a depth of 30 microns, forming crater-like areas of demineralization containing odontoblast processes, uncovered collagen fibers. Under natural conditions, dentinal fluid serves to hold the network of collagen fibers, occupying all the free space between the fibers, forming a microscopic relief of the dentin.
Etching Techniques
The following tooth tissue etching techniques are distinguished:
- total etching;
- selective etching;
- use of self-etching adhesive.
Fundamental concepts that have become widespread in dentistry:
- "wet" bonding – this is total etching,
- "dry" bonding – this is a self-etching technique or selective etching technique.
The first implies complete removal of water from the enamel surface, but it is important to keep the dentin moist, glossy, and shiny to prevent the collapse of collagen fibers.

Figure 3. Selective etching.
The second involves complete removal of moisture from the surface, enamel, and dentin. Additionally, the dentin surface is treated with moisturizers, which hydrate and stabilize the collagen fiber network.
Total Etching Technique
This technique involves just one step: an etching agent is applied to all surfaces of the enamel and dentin, resulting in the total removal of the "smear" layer, and demineralization of the superficial layers of the dentin.
Selective Etching Technique
Includes several steps:
- initially, the enamel surface is treated with an etching agent, it is allowed to set for some time and then rinsed off with a water spray;
- then a primer is applied, which includes an etching agent or a self-etching adhesive.
In the process of this technique, the "smeared" layer is modified, transformed into a hybrid layer, there is no collapse of collagen fibers and movement under the influence of odontoblast process dentinal fluid inside the dentinal tubules. Dentinal tubules are sealed by the hybrid layer, which helps to level the degree of postoperative sensitivity. Additionally using phosphoric acid for etching before applying the universal adhesive significantly enhances the bond of the adhesive with the enamel of the tooth, but such an effect is not observed on dentin.
The "all-in-one" technique
Involves the use of a self-etching adhesive in one step, a liquid that includes molecules of the etching agent, hydrophobic and hydrophilic components, which provides modification of the "smeared" layer.
The primer applied to the dentin surface provides hydration of the gaping dentinal tubules, rids them of excess moisture. The HEMA monomer – a component of the primer, helps the hydrophobic molecules of the adhesive penetrate the network of collagen fibers, reopens and expands it, increases the strength and bonding area with the adhesive.
HEMA in dentin moisturizers is found in complex with substances that contribute to the stabilization of collagen fibers (salicylates, glutaraldehyde).
The adhesive ensures the filling of interfibrillar voids formed as a result of the opening of the collagen fiber network. Encapsulation of the latter occurs as a result of the dissolution or transformation of the smeared layer, which causes the formation of a hybrid layer, represented by the adhesive, hydroxyapatite crystals, collagen, acting as an insulating pad, preventing the centrifugal movement of dentinal fluid in the dentinal tubules, which ensures a reduction in the degree of postoperative sensitivity.
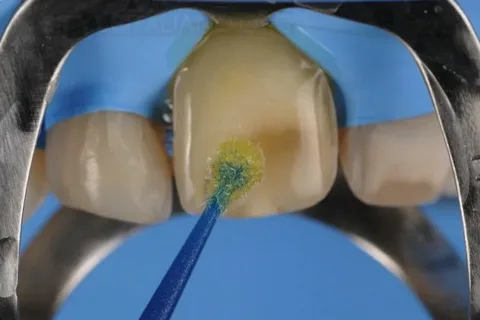
Figure 5. Applying the adhesive.
A universal adhesive system is the best choice in the vast majority of clinical situations, simplifying the work of the dentist, and ensuring long-term adhesion of the composite restoration over an extended period in the oral environment.
The characteristics of systems used in total-etch techniques significantly differ from the properties of self-etch systems. Each system has its own positive and negative qualities, which is important when assessing indications for their use.
Learn more about this topic in the webinar Modern Approach in Adhesive Orthopedic Dentistry.