Candidal Stomatitis: Etiology, Symptoms, Diagnosis
Machine translation
Original article is written in RU language (link to read it) .
Candidal stomatitis, oral candidiasis, candidiasis of the oral mucosa, and in layman's terms - thrush - are all synonyms for the same disease, caused by yeast-like fungi. This article will discuss the etiology, symptoms, and diagnosis of candidal stomatitis.
For more useful information on diseases of the oral mucosa, visit our website section Learning in Periodontology.

Etiology of Candidal Stomatitis
The cause of candidal stomatitis is yeast-like fungi of the genus Candida. These fungi are classified as imperfect fungi, deuteromycetes, which have a complex structure. They have a cell wall consisting of 5-6 layers, a perforating organ that affects host cells, and they have significant differences compared to other yeast-like fungi.
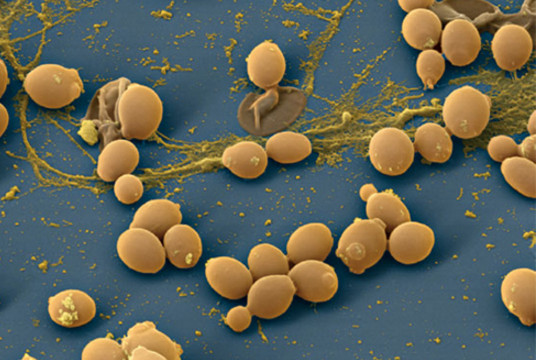
The differences between Candida fungi and other yeast-like fungi are as follows:
- ability to grow in environments with temperatures of 30-37 degrees Celsius;
- optimal environment — mildly acidic/acidic (pH = 5.8 – 6.5);
- ability to ferment carbohydrates (main source of nutrition);
- aerobes (oxygen-loving);
- prefer environments with glycogen.
Candida species are opportunistic pathogens, meaning that in the absence of predisposing factors, they are safe. However, as soon as changes occur in this balance, they become pathogenic. It is important to understand which specific conditions lead to the activation of pathogenicity in Candida fungi. Here, the main role is not played by pathogenic factors, but by the state of the human immune defense. Of course, the pathogenicity of Candida species varies between animals and humans. For humans, Candida albicans is the most dangerous, and for children – Candida tropicalis.
Predisposing Factors for Candidal Stomatitis
The factors that contribute to the activation of pathogenic factors by Candida are as follows:
- decreased body's defense mechanisms – immunity;
- presence of congenital or acquired immunodeficiencies;
- metabolic disorders, endocrine disorders (diabetes, amenorrhea, iron deficiency conditions);
- avitaminosis (especially of vitamins B1, B2, B12, which are involved in suppressing the action of microorganisms);
- acute infectious diseases, exacerbations of chronic diseases;
- diseases of the female reproductive organs;
- prolonged use of oral contraceptives;
- pregnancy;
- large burns;
- rickets;
- prematurity;
- oncology;
- diseases of the gastrointestinal tract;
- use of antibiotics, large doses of drugs, immunosuppressants;
- working conditions. It has been noted that people working in hydrolysis-yeast plants, antibiotic production plants, breweries, and other alcoholic beverage factories are more likely to suffer from candidal stomatitis;
- failure to observe personal hygiene rules;
- failure to maintain cleanliness and order in household items (Candida can be found on children's toys, plates, cups);
- consumption of unwashed vegetables, fruits;
- in breastfed infants, candidal stomatitis most often occurs when they are overheated, i.e., wearing tight pajamas, bulky swaddling.
- artificial feeding of children up to 6 months;
- iatrogenic factors: sharp edges of fillings, improperly fitted dental prostheses, chemical burns with formalin, arsenic pastes. Anything that leads to disruption of the integrity of the oral mucosa.
As can be seen, there are many reasons and factors for the activation of candida. Therefore, the approach to treatment must be adequate, and the cause should be treated first, and then the manifestations.
Pathogenesis of Candidal Stomatitis
The pathogenesis of candidal stomatitis is quite simple: the fungus is located on the surface of the oral mucosa or on the skin surface, and in the absence of damage or provoking factors—it does not penetrate inside the epithelium; if present, it penetrates and visible pathology begins.
However, these are only two of the five mechanisms of action of fungi on the body. Candidiasis is a very serious problem, as it is capable of spreading to organs. Thus, after penetrating the epithelium, candida can interact with macrophages and neutrophils. After which it penetrates into the cells of such organs as the liver, heart, kidneys - granulomas are formed. And the last and most ominous stage is penetration into the blood and the development of candidemia. After which death occurs.
Classification of Candidal Stomatitis
Classification of candidal stomatitis according to ICD-10:
- A00-B99 Certain infectious and parasitic diseases;
- B35-B49 Mycoses;
- B37 Candidiasis
- B37.0 Candidal stomatitis - oral thrush.
Classification of candidal stomatitis by N.D. Sheklakov:
- Superficial candidiasis of mucous membranes, skin, nails;
- Chronic generalized (granulomatous) candidiasis;
- Visceral (systemic) candidiasis.
By course:
- Acute pseudomembranous candidiasis (thrush);
- Acute atrophic candidiasis;
- Chronic hyperplastic candidiasis;
- Chronic atrophic candidiasis.
Symptoms of candidal stomatitis
Symptoms of candidal stomatitis:
- pain during eating;
- pain at rest;
- burning sensation;
- itching;
- dryness of the mouth;
- unpleasant mouth odor;
- presence of spots on the mucous membrane;
- distortion (alteration) of taste;
- bleeding gums;
- enlargement of lymph nodes;
- increase in body temperature.
Sores are most commonly found on the mucous membranes of the cheeks, palatine tonsils, and the inner side of the lips. They are least common on the tongue and under the tongue.
Diagnosis of Candidal Stomatitis
The diagnosis of candidal stomatitis will be based on patient interview and clinical examination by a specialist. In addition, to confirm the diagnosis of CANDIDAL stomatitis, laboratory diagnostics are necessary. For this, a swab (smear) is taken from the surface and sent to the laboratory. In the laboratory, the materials are examined in 2 directions:
- cultures on nutrient media — Sabouraud's medium, wort-agar or candida-agar;
- microscopy of stained smears.

The presence of 300 colonies in 1 ml indicates candida carriage. Detection of a higher number of colonies in the initial culture suggests candidiasis. However, the diagnosis is confirmed only with a repeat culture and when the numbers are higher than 300 colonies per 1 ml.
Acute Pseudomembranous Candidiasis
Acute pseudomembranous candidiasis is the most common form of mucosal candidiasis of the oral cavity. It is acute pseudomembranous candidiasis that is known as thrush, not other types of candidiasis. Infants and weakened adults are more often affected.
Symptoms of acute pseudomembranous candidiasis:
- complaints of a child refusing to feed;
- children are lethargic and fussy;
- complaints of pain when eating, burning and dryness in the mouth.
Clinical presentation of acute pseudomembranous candidiasis:
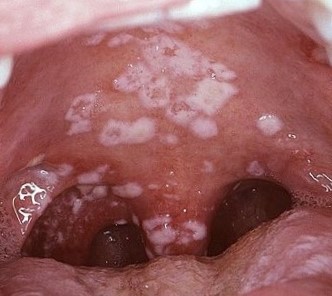
On the mucous membrane of the oral cavity - white or blue-white spots, coating resembling "curd-like masses", which when scraped off leave a reddened surface. In other cases, the coating is difficult to scrape off, bleeds, revealing an eroded surface. The process often affects the tongue, palate, lips, but can spread to the pharynx, larynx, and esophagus. Without treatment, acute pseudomembranous candidiasis progresses to acute atrophic candidiasis.

Acute Atrophic Candidiasis
Symptoms of Acute Atrophic Candidiasis
- complaints of dryness and burning in the mouth;
- pain while chewing, during conversation;
- inability to open the mouth widely;
- complaints of scales on the lips;
- dryness and cracks on the lips.
Clinic of Acute Atrophic Candidiasis
The clinic of acute candidal stomatitis differs from the clinic of acute pseudomembranous candidiasis by the ABSENCE of plaque.
In acute atrophic candidiasis, the mucosa is hyperemic, fiery, and also dry, which complicates the opening of the mouth. There is no plaque. On the tongue, there is papillary atrophy (i.e., smoothness of the pattern), the tongue is smooth and bright red. There may be teeth marks on the tongue. The red border of the lips is hyperemic, dry, with the presence of gray scales. In the corners of the lips – cracks and erosions.


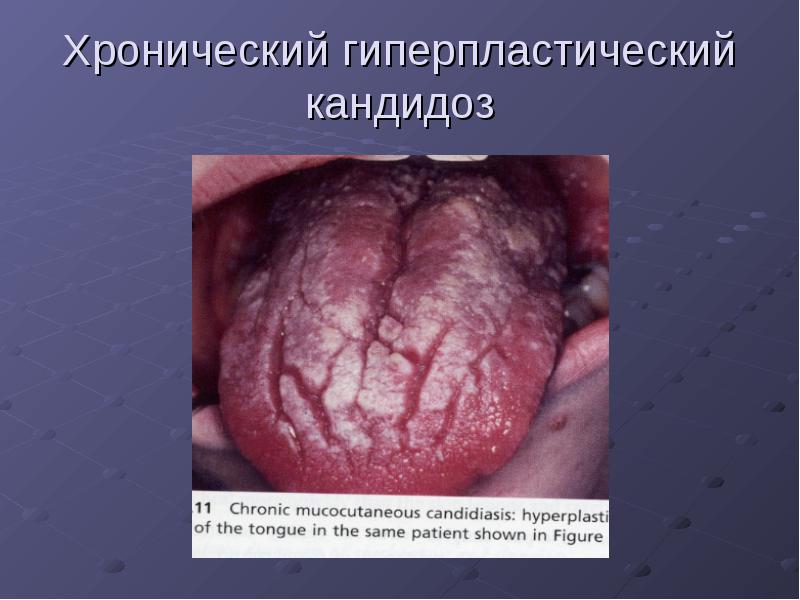
Chronic Hyperplastic Candidiasis
Symptoms of Chronic Hyperplastic Candidiasis
- complaints of pain when consuming spicy, hot food;
- distortion (change) of taste;
- burning sensation in the mouth.
Clinic of Chronic Hyperplastic Candidiasis
On the hyperemic mucosa, the appearance of plaques ("cobblestone pavement") is noted. The plaques are gray-white, tightly adhered to the mucosa, which when removed leads to bleeding and pain. They are most often found on the back of the tongue. They can spread to the tonsils, pharynx, throat, and esophagus.
Chronic Atrophic Candidiasis
Chronic atrophic candidiasis is most often diagnosed in patients with dental prostheses.
Symptoms of Chronic Atrophic Candidiasis
- complaints of burning sensation;
- complaints of pain when eating;
- complaints of dry mouth
Clinic of Chronic Atrophic Candidiasis
The mucosa under the prosthetic bed is swollen and hyperemic. In some areas, there is a white coating that is easily removable. Upon removal of the white coating – the surface is hyperemic. In the corners of the mouth – erosions covered with a white coating. Tongue lesions may be noted: the tongue is smooth, papillae are atrophied, and there are teeth imprints on the tongue. In some cases, hypertrophy of the filiform papillae is noted – "black hairy tongue".
Treatment of Candidal Stomatitis
The treatment of candidal stomatitis must be strictly individual. Since candidal stomatitis is often a secondary disease, it is essential to first identify and eliminate the cause.
The treatment of candidal stomatitis should be both systemic and local.
Systemic treatment of candidal stomatitis includes:
- prescribing general strengthening therapy;
- prescribing antifungal medications;
- prescribing a diet that excludes sweets and other carbohydrates. The food should be rich in fiber.
Polyene antibiotics are preferred, as they are the primary means for treating candidal stomatitis. Examples of such drugs include nystatin and levorin (it is advisable to dissolve the tablet and discard it, as polyene antibiotics are poorly absorbed by the body). Polyvitamin complexes with B vitamins, calcium, and iron are also prescribed. Desensitizing therapy with drugs like diphenhydramine and suprastin is also conducted.
Local treatment of candidal stomatitis involves:
- application of mucous membranes with polyene antibiotics in the form of solutions or ointments for 14 days, 3-4 times a day;
- prescription of alkaline applications with 2-4% sodium bicarbonate solution;
- thorough sanitation of the oral cavity, professional hygiene, replacement of old and irrational orthopedic structures.
Prevention of candidal stomatitis
Prevention of candidal stomatitis includes:
- proper prescription and use of antibiotics, antidepressants;
- timely treatment of diseases;
- planning of pregnancy;
- thorough cleaning of rooms;
- consumption of only washed vegetables and fruits, fresh meat and dairy products;
- visiting the dentist at least once every six months;
- mothers should ensure clean nipples, bottles for their babies, and not neglect hygiene.
On our website you will always find a lot of relevant information on various sections of dentistry.
