Difficult teething
Machine translation
Original article is written in RU language (link to read it) .
First, let's consider what an impacted tooth is. It is a fully developed and formed tooth that is located not in the dental arch, but within the thickness of the jawbone tissue, and has not erupted on time. Often, impacted teeth are supernumerary teeth. Unlike retention, semi-retention is a condition where the tooth has erupted in the jaw but is still located under the mucosal cap.
The differences between an impacted tooth and a tooth in the bone are presented in the webinar Impaction of teeth: causes of development, anatomical prerequisites, tools and operation techniques.
Partial retention is recognized if the eruption process has stopped, and only a small part of the crown has managed to emerge from the socket. There is also a concept of difficult eruption, which is observed at inappropriate times, due to certain anatomical prerequisites (features of topography) or undetermined etiology.
Classification Principles
Retention by type is subdivided into:
- wisdom teeth,
- upper canines,
- lower premolars,
- second lower molars in adolescents.
The following varieties of dystopia of retained teeth are distinguished:
- mesioangular;
- horizontal;
- vertical;
- buccal.
- lingual;
- distoangular;
- inverse (inverted position);
- unusual.
Types of retention depending on the area adjacent to nearby teeth:
- the crown is adjacent to the crown;
- the crown is adjacent to the neck;
- the crown is adjacent to the root.

Figure 1. Difficult eruption of wisdom teeth.
Etiology of Difficult Eruption
The causes of difficult eruption are diverse, but they can all be grouped into the following main categories:
- delay in growth and development of the jawbone tissue;
- immaturity, underdevelopment of muscle fibers and structures of the dental-jaw system;
- late eruption of permanent teeth;
- characteristics of the dental follicles placement in the embryonic period;
- atypical process of resorption of the roots of deciduous teeth;
- characteristics and dietary habits (lack of hard food, predominance of high-carbohydrate products);
- untimely, non-physiological replacement of milk teeth.
Clinical Manifestations and Diagnostic Principles
Difficult eruption can occur almost asymptomatically, not accompanied by clinical symptoms of inflammation. Often such teeth are discovered accidentally during radiological examination. In such cases, radiologically, the following will be observed:
- presence of an impacted tooth in the jawbone, which is located within the bone;
- the X-ray can assess its relation to adjacent teeth;
- changes in bone mass may be observed around the impacted tooth.
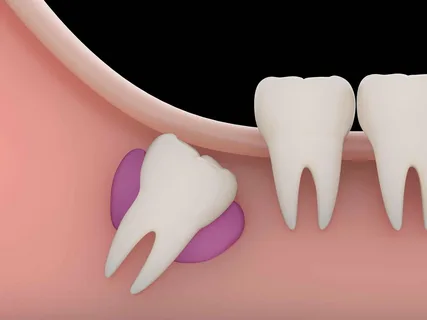
Figure 2. Inflammatory changes in the area of the impacted tooth.
Difficult eruption may be accompanied by inflammatory phenomena, then it is important to assess the combination of factors:
- presence of erupted cusps, their number;
- position of the tooth;
- severity of inflammation symptoms;
- presence of pus discharge from under the mucosal "hood";
- changes from the surrounding tissues (adjacent gum, mandibular lingual groove, transitional fold, retromolar triangle), pain in this area, presence of infiltrates;
- when joining the contracture of the masticatory muscles, the degree of its severity is determined;
- difficulty and pain when swallowing;
- radiologically assess: presence of an unerupted tooth, its position in the bone, relation to adjacent teeth, disturbances in the bone around the unerupted tooth.
Complications
Retained teeth can remain in the jaw for a long time without causing any discomfort to the patient, or they can cause a number of complications, among which the following can be highlighted:
- neuralgia, which develops due to compression of the nerve endings of n. Trigemini or as a result of complications of caries of the unerupted tooth itself;
- a follicular cyst may form;
- inflammatory processes in the surrounding tissues (phlegmons, abscesses, osteomyelitis);
- deformation of the jaws, which is accompanied by the formation of a pathological bite.
Treatment
The principles of therapy for retained teeth depend on the course of the disease. If retention does not accompany inflammatory phenomena, in such cases, if there are no complaints about cosmetic or functional disorders, surgical interventions are not required. The patient is recommended dynamic observation.
If retention is accompanied by inflammatory phenomena, and the patient is diagnosed with incomplete retention, pericoronitis against the background of no significant radiological disturbances near the retained tooth, then surgical excision of the mucosal "hood" is indicated.

Figure 3. Development of pericoronitis.
Course of the surgical intervention. The mucosa over the occlusional surface of the unerupted tooth is excised, and the distal edge is freed to prevent recurrence.
If pericoronitis is clinically determined against the background of incomplete retention with significant radiological signs of pathology near the retained tooth, in such cases, in addition to the excision of the mucosal "hood," surgical extirpation of the partially retained tooth with subsequent wound revision is indicated.
In the case of complete retention, accompanied by significant inflammatory phenomena, which are confirmed during clinical and radiological examination, it is necessary to perform a surgery for the complete removal of the retained tooth by an open method.
Types of surgeries for retained teeth
- Closed extirpation with forceps of a partially retained tooth, most often performed for the retention of upper canines, lower and upper wisdom teeth, with simultaneous excision of the mucosal "hood" if present.
- Closed extirpation with an elevator of a partially retained tooth, most often performed for the retention of lower third molars, with excision of the mucosal "hood" or if it is present.
- Open extirpation of the retained tooth entirely without dividing it into parts.
- Open extirpation of the unerupted tooth with division into fragments (odontectomy).
Closed extraction of a partially impacted tooth using forceps (for upper canines, all wisdom teeth) involves a preparatory stage, adherence to protocol, and postoperative patient management, with no differences from the generally accepted technique of closed tooth extraction. It is only important to consider some features: significant remoteness of the operational field, unsatisfactory view, morphological nuances of the alveolar process, proximity to the maxillary sinus above, and to the angle and branch of the jaw below, frequent traumatization of the mouth corners, difficulties associated with applying forceps along the tooth axis.
Closed extraction of a partially impacted lower wisdom tooth using an elevator. The removal technique is similar to that using forceps. It is important to assess the stability and integrity of the second molars, so they can be relied upon during the operation.
Open extraction of an impacted tooth entirely without dividing it into parts is performed according to the protocol for complex removal, which involves forming a mucoperiosteal flap, osteotomy, and osteoectomy of a fragment of the external cortical plate in the area of the impacted tooth, from which the tooth located in the bone is extracted through the formed window in the alveolar process.
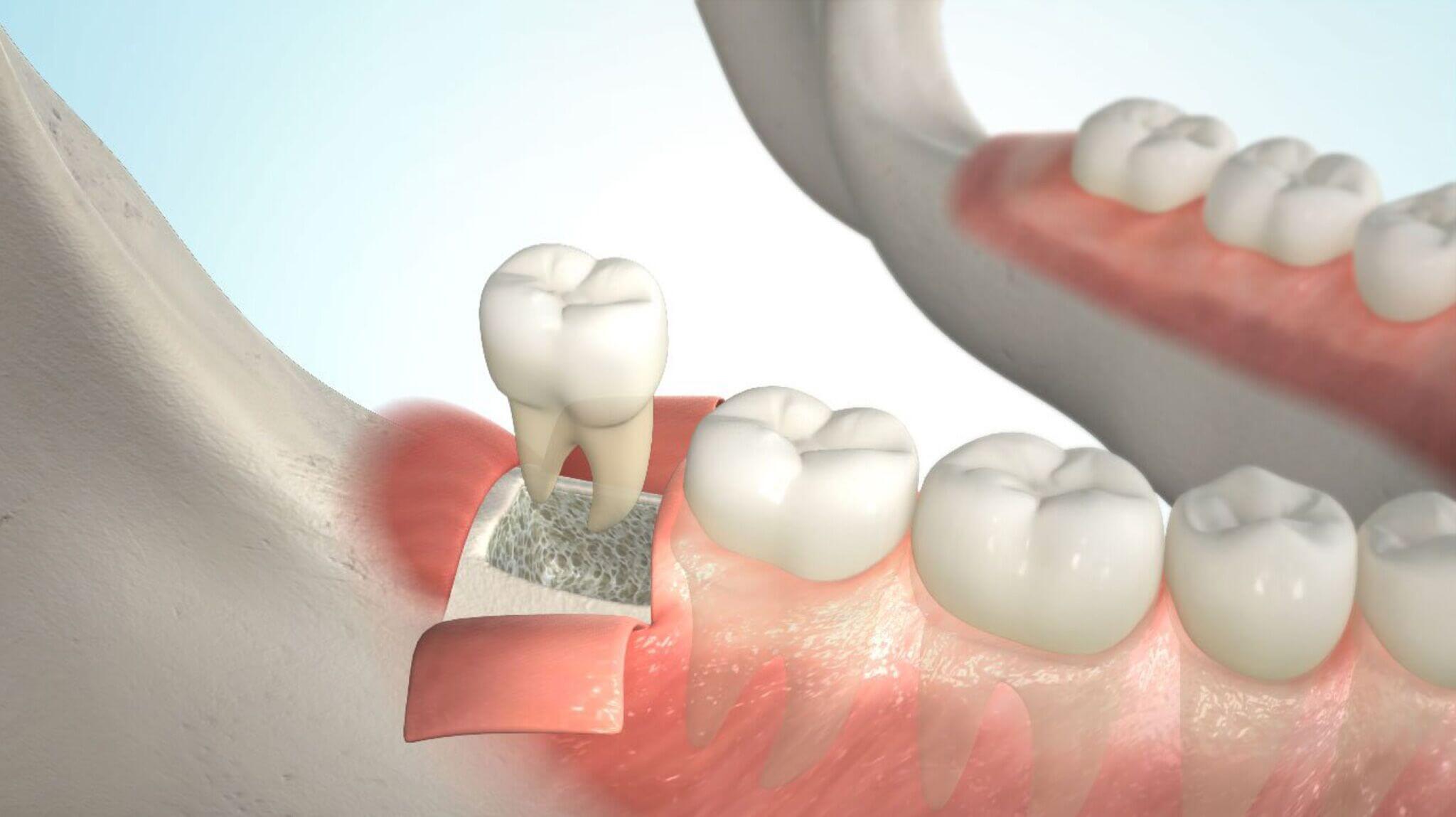
Figure 4. Open removal of an impacted tooth.
Open extirpation of an unerupted tooth with division into fragments (odontectomy) is performed if it is impossible to extract the tooth as a whole or there is a high risk of complications:
- fracture of the bone in the area of the body or angle of the lower jaw as a result of removing a significant bone fragment;
- damage to the fibers of the inferior alveolar nerve;
- perforation of the maxillary sinus;
- pushing the tooth being removed into the soft tissues;
- damage to adjacent teeth.
The following odontectomy techniques are distinguished:
- Division of only the crown of the tooth being removed.
- Division of both the crown and the root.
Complications
Complications may be directly related to the presence of an unerupted tooth, or may develop as a result of its removal in the postoperative period.
Complications associated with the presence of an unerupted tooth in the bone:
- pericoronitis,
- caries or its complications of the impacted tooth itself or the contact surface of the second molar,
- periodontitis,
- periostitis,
- abscess,
- phlegmon,
- root resorption of adjacent teeth as a result of compression by the impacted tooth,
- follicular cysts,
- neoplasms (ameloblastoma), their formation is associated with improper formation of the enamel organ (rarely encountered).
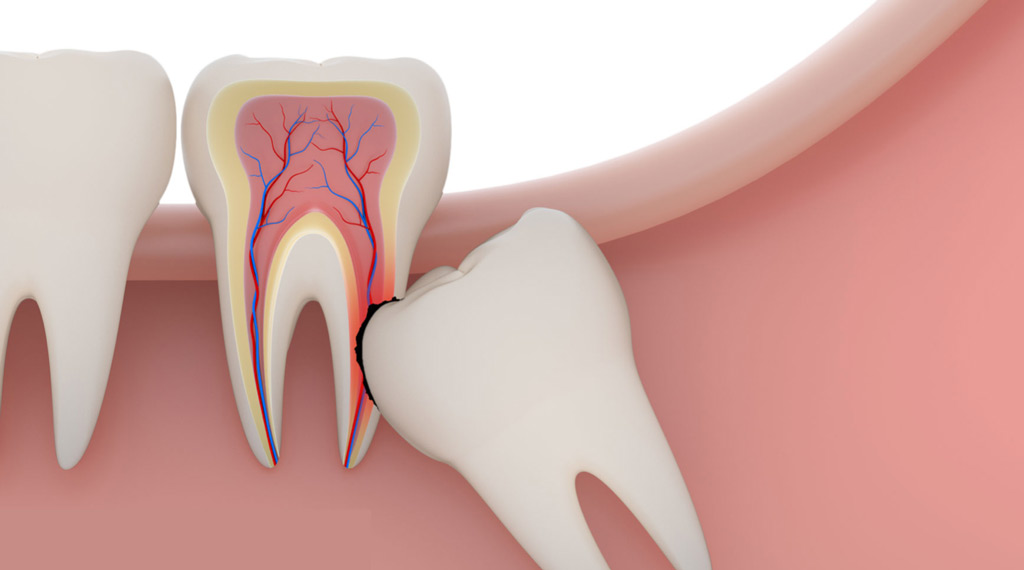
Figure 5. Resorption of the adjacent tooth.
Possible postoperative complications:
- nerve damage,
- fracture of the lower jaw,
- perforation of the floor of the maxillary sinus,
- pushing the tooth into the soft tissues,
- traumatic damage to adjacent teeth,
- prolonged healing and pain of the postoperative wound,
- socket osteomyelitis, alveolitis,
- abscess, phlegmon.
Detailed protocols for removing wisdom teeth on the upper and lower jaws are presented in the online course Complex Removal of 8th Teeth.
